Benign Prostate Hypertrophy (BPH):
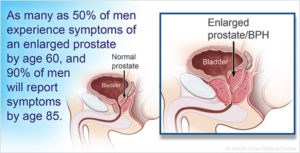
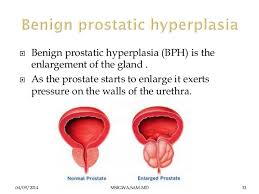
What is this? Benign prostatic hyperplasia (BPH) is a health issue that becomes more common with age. It’s also called an enlarged prostate. The prostate is a small gland that helps make semen. It’s found just below the bladder. And it often gets bigger as you get older.
Sexual health is a major overall health marker for men — 1 in 4 men will experience some form of sexual health concern by age 65.
Erectile dysfunction and lower testosterone are linked to larger health risks, including heart disease, high blood pressure-HBP, diabetes and obesity. Remember African Americans are high for blood pressure. Perhaps higher rates of obesity and diabetes place African Americans at greater risk for high blood pressure and heart disease. Researchers have also found that there may be a gene that makes African-Americans much more salt sensitive. This trait increases the risk of developing HBP. In people who have this gene, as little as one extra gram (half a teaspoon) of salt could raise blood pressure as much as five millimeters of mercury (mm Hg). Don’t forget bad diet, overweight to obese and sedentary life style play vital factors for getting HBP so on average it’s not just a gene factor but heredity does key in especially if you have disease (DM, Obese, Cardiac disease with HBP in the nuclear family especially).
Diet and medicine can control symptoms. You will have a yearly exam. Your health care provider will look for worse or new symptoms before beginning active treatment.
Why go to your health care provider? He will do a yearly exam looking for worse or new symptoms before beginning active treatment. Who should do this? Good candidates which are men with mild signs and symptoms of BPH, There are no side effects in having your doctor check you out. Just remember avoidance to the M.D. may make the situation to be harder to reduce your symptoms later on for not going to the M.D. yearly.
The causes of benign prostatic hyperplasia – (BPH)
The cause of BPH is not well understood; however, it occurs mainly in older men. Benign prostatic hyperplasia does not develop in men whose testicles were removed before puberty. For this reason, some researchers believe factors related to aging and the testicles may cause benign prostatic hyperplasia.
Throughout their lives, men produce testosterone, a male hormone, and small amounts of estrogen, a female hormone. As men age the amount of active testosterone in their blood decreases, which leaves a higher proportion of estrogen. Scientific studies have suggested that benign prostatic hyperplasia may occur because the higher proportion of estrogen within the prostate increases the activity of substances that promote prostate cell growth.
Another theory focuses on dihydrotestosterone (DHT), a male hormone that plays a role in prostate development and growth. Some research has indicated that even with a drop in blood testosterone levels, older men continue to produce and accumulate high levels of DHT in the prostate. This accumulation of DHT may encourage prostate cells to continue to grow. Scientists have noted that men who do not produce DHT do not develop benign prostatic hyperplasia.
Risk factors include aging and a family history of BPH. Other risk factors are obesity, lack of physical activity, and erectile dysfunction (ED).
Preventions Measures of Benign Prostate Hypertrophy – BPH:
There is no sure way to prevent BPH. Because excess body fat may affect hormone levels and cell growth, diet may play a role. Losing weight and eating a healthy diet, with fruits and vegetables, may help prevent BPH. Staying active also helps weight and hormone levels.
With BPH, the prostate gets larger. When it is enlarged, it can irritate or block the bladder. A common symptom of BPH is the need to urinate often. This can be every one to two hours, especially at night.
Symptoms of Benign Prostate Hypertrophy (BPH):
- Feeling that the bladder is full, even right after urinating
- Feeling that urinating “can’t wait”
- Weak urine flow
- Dribbling of urine
- The need to stop and start urinating several times
- Trouble starting to urinate
- The need to push or strain to urinate
In severe cases, you might not be able to urinate at all. This is an emergency. It must be treated right away. It is foolish for someone to not get checked or treated since the condition like any other disease left untreated will only worsen and in time possibly kill you (Ex. CHF OR Diabetes OR even Obesity).
How Can BPH Affect Your Life?
In most men, BPH gets worse as you age. It can lead to bladder damage and infection. It can cause blood in the urine. It can even cause kidney damage. Men with BPH should get treated. Mild cases of BPH may need no treatment at all. In some cases, minimally invasive procedures that do not require anesthesia are good choices. And sometimes a combination of medical treatments works best.
BPH is monitored by your doctor and there are active treatments.
Treatments to Benign Prostate Hypertrophy -BPH:
Medications are often the first treatment for BPH. There are two types of medications that may be prescribed.
- Alpha-Blockers: This type of medication relaxes the muscles in the prostate and bladder neck, which helps urine flow better. Tamsulosin and alfuzosin are common alpha blockers often used as the first line of defense against BPH symptoms. They can provide relief for many individuals.
- 5-Alpha Reductase Inhibitors: These medications target the hormones (dihydrotestosterone) that cause the prostate to grow. Finasteride and dutasteride are common examples of these medications, which slow the growth of the prostate and improve urinary symptoms over time.
- Combination Therapy: In some cases, your physician may prescribe a combination of alpha-blockers and 5-alpha reductase inhibitors for a combined effect, offering both immediate relief and long-term benefits.
While medications can be effective in treating an enlarged prostate, some individuals may not be able to tolerate their side effects. Those may include lightheadedness, dry mouth, low blood pressure, falls, headaches, erectile dysfunction, retrograde ejaculation, reduced libido, nausea, or vomiting. If these occur and become burdensome, talk to your doctor so other treatment options can be explored.
Surgeries:
Transurethral resection of the prostate (TURP) is a type of prostate surgery done to relieve moderate to severe urinary symptoms caused by an enlarged prostate, a condition known as benign prostatic hyperplasia (BPH).
During TURP, a combined visual and surgical instrument (resectoscope) is inserted through the tip of your penis and into the tube that carries urine from your bladder (urethra). The urethra is surrounded by the prostate. Using the resectoscope, your doctor trims away excess prostate tissue that’s blocking urine flow and increases the size of the channel that allows you to empty your bladder.
TURP is one of the most effective options for treating urinary symptoms caused by BPH.
There are other forms of surgeries There are several types of minimally invasive procedures to choose from, they include:
- Prostatic Stent
- High Intensity Focused Ultrasound (HIFU)
- Holmium Laser Enucleation of Prostate (HoLEP)
- Interstitial Laser Coagulation (ILC)
- Transurethral Electroevaporation of The Prostate TUVP
- Transurethral Microwave Thermotherapy (TUMT)
- Transurethral Needle Ablation (TUNA)
- Photoselective Vaporization (PVP)
- UroLift
- Catheterization
- How do you know which is best for you GO to the M.D. (Urologist), whose the expert in making that decision. Guess what guys? Many less invasive procedures can be done right in the doctor’s office. So go find out if you’re having symptoms of BPH!
- How do you know which is best for you GO to the M.D. (Urologist), whose the expert in making that decision. Guess what guys? Many less invasive procedures can be done right in the doctor’s office. So go find out if you’re having symptoms of BPH!