

The corona virus spreads continues to grow around the globe, there are steps you can take to protect yourself and your family.
“I told my children that while I didn’t think that they were at risk right now, we, as a family, need to be preparing for significant disruption of our lives,” says Dr. Nancy Messonnier of the Centers for Disease Control and Prevention.
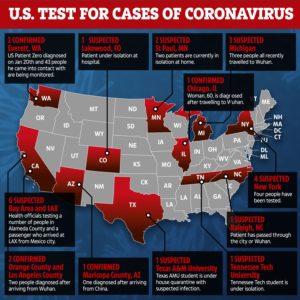
The CDC plans to expand testing across the U.S. as a preventative measure.
Currently, if you live in the U.S. the risk of getting the virus remains very low, but public health officials say there will likely be outbreaks in the United States. So this is a good time to review your emergency game plan.
Here’s what you need to know to make good decisions to plan, prepare and even prevent the spread of the disease.

Prepare Home with Goods and Storage:
1. This virus is contagious, but it’s not as deadly as other outbreaks
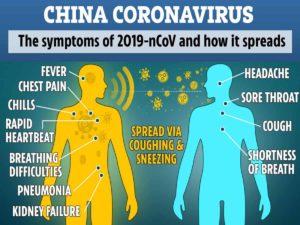
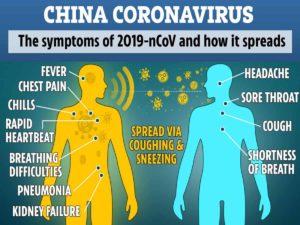
In China, more than three quarters of the cases have been classified as mild. Symptoms include low-grade fever and a cough. Some people also experience fatigue, headaches and, less frequently, diarrhea.
Overall, the death rate in China is estimated at 2 percent, and the average age of death among those with COVID-19 is in the 70’s. People with underlying medical problems, and particularly smokers, seem to be at higher risk.
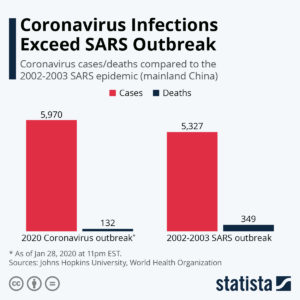
Compared to prior outbreaks of novel viruses, this coronavirus appears less deadly than other human coronaviruses that have spread in recent years. For instance, the death rate was about 34% for MERS, and about 10% for SARS.
The flu causes more than 12,000 deaths a year in the U.S. An annual vaccine is the most effective way to prevent flu, but there are other strategies to prevent it. So far, there’s no vaccine against the new coronavirus, but some of the same strategies to prevent flu can also protect against coronavirus.
2. To fend off coronavirus, follow flu prevention tips
The top tip: Wash your hands. Why? Viruses can spread from person to person via respiratory droplets. When an infected person coughs or sneezes, close contacts can be infected. In addition, the virus can end up on door knobs, elevator buttons and other surfaces. If you touch those surfaces then touch your eyes, nose or mouth, you can become infected.
This is why it’s important to wash rigorously. Here’s the CDC’s guidance.
“Wash your hands often with soap and water for at least 20 seconds, especially after going to the bathroom; before eating; and after blowing your nose, coughing, or sneezing.”
“Americans are friendly. We not only shake hands, we also hug. These are ways we can transmit the virus,” Katz says. She recommends an elbow bump.
Here’s 5 more things to remember, per the CDC:
- Avoid close contact with people who are sick.
- Avoid touching your eyes, nose, and mouth.
- Stay home when you are sick.
- Cover your cough or sneeze with a tissue, then throw the tissue in the trash.
- Clean and disinfect frequently touched objects and surfaces using a regular household cleaning spray or wipe.
3. Don’t panic — start to prepare
This is not the time to panic, but it is a time to prepare – good old fashioned preparedness planning for your family,” says Rebecca Katz, who directs the Center for Global Health Science and Security.
Think about the threat of a possible outbreak in your community the way you’d think about a big snowstorm or a hurricane. If it never hits, great. But if it does, you’ll be glad you prepared.
Don’t hoard, but do stock your cupboards with some extra food and cleaning supplies. Each time you grocery shop, buy a few extra items. Shelf stable foods such as beans and rice are good options. Also, utilize your freezer to preserve foods, everything from meats and vegetables to cooked grains and bread. Think about having enough on hand to last a few weeks.
- Check the medicine cabinet to ensure you have basic medications such as aspirin or ibuprofen.
- Think about a back up plan if schools were to close during an outbreak.
- If you take a daily prescription medication, have as much of a supply on hand as possible.
- Ask your employer about a work-from-home option.
“If there’s widespread virus in your community, you may not want to go to the [store]. You may want to distance yourself from others,” Katz says.
4. The uncertainty of masks to prevent illness
Overall, there’s not conclusive evidence that wearing a face mask can help prevent people from being infected by the virus. And public health officials give mixed messages about usefulness for the general public. As we’ve reported, masks may not fit the face tightly, so you’re still able to breath in infected droplets. And, experts worry that masks can give a false sense of security.
Health care providers are trained to use masks properly, and there’s evidence that they’re effective in clinical settings. For people at home, the CDC recommends using masks in certain situations. For instance, if you’re caring for an infected person at home, the proper use of masks can protect the caregiver.
5. Be smart about travel
The CDC updates its travel advisory information frequently. The federal government uses a 4 level scale to rank risk. Level 1 = lowest risk, Level 4, highest.
For Italy, where there’s been sustained spread of the novel coronavirus, there’s now a Level 2 Alert. The CDC advises that older adults and those with chronic medical conditions should consider postponing nonessential travel. “Travelers should avoid contact with sick people and clean their hands often by washing with soap and water for at least 20 seconds or using an alcohol-based hand sanitizer with 60%–95% alcohol.”
Check your health insurance to see if it includes international travel coverage, the CDC recommends. Also, consider travel health insurance and medical evacuation insurance.
The CDC estimates that — without insurance, a medical evacuation can $100,000 or more.
If you’ve planned a cruise or overseas travel consider the possibility of travel disruptions in the event of an outbreak. “Think about the consequences of being caught on ship or over a border when decisions are being made,” that could limit or disrupt your travel without much warning says Christopher Mores of George Washington University. If you were quarantined, what would your back-up plan be for your work and family responsibilities back home? This is definitely something to consider.