Archive | October 2018
QUOTE FOR TUESDAY:
“Candy corn was invented in the 1817 and designed to mimic the appearance of a kernel of corn, but was made from wax, sugar, and corn syrup. The only problem? It really does just taste like wax, sugar, and corn syrup. Candy companies now sell their extra yearly inventory to Third World Countries, who use it to pave roads.”
USA Today
QUOTE FOR MONDAY:
“While scientists do not know what exactly causes psoriasis, we do know that the immune system and genetics play major roles in its development. Usually something triggers psoriasis to flare. The skin cells in people with psoriasis grow at an abnormal fast rate, which causes the buildup of psoriasis lesions.”
National Psoriasis Foundation
QUOTE FOR THE WEEKEND:
“Spina bifida is a condition that affects the spine and is usually apparent at birth. It is a type of neural tube defect (NTD).”
Centers for Disease Control and Prevention (CDC)
QUOTE FOR FRIDAY:
“The immediate cause of sudden cardiac arrest is usually an abnormality in your heart rhythm (arrhythmia), the result of a problem with your heart’s electrical system.”
MAYO CLINIC
QUOTE FOR THURSDAY:
“Sudden Cardiac Arrest (SCA)is the leading cause of death in the United States, taking the lives of more than 350,000 people each year. Anyone can experience Sudden Cardiac Arrest (SCA), including infants, children, teens, young adults and people in their 30s and 40s who have no sign of heart disease, as well as more mature adults. SCA is not a heart attack.”
stopcardiacarrest.org
QUOTE FOR WEDNESDAY:
“Heart attacks can be deadly, and the widow maker is one of the deadliest kind. You most likely won’t survive.”
Web M.D.
QUOTE FOR TUESDAY:
“Always put your baby to sleep on his back. Use a pacifier at sleep time. Ury swaddling your child. Have her sleep in a crib in your room. Make sure the crib mattress is firm and tight-fitting.”
PARENTS (wwwParents.com)
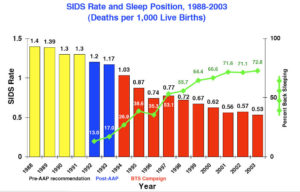
How to help in preventing SIDS–safe environment for your baby for the first step!
1. Place your baby on his or her back for all sleep times—for naps and at night. Some parents may be concerned that a baby who sleeps on his or her back will choke if he or she spits up during sleep. However, babies’ anatomy and gag reflex will prevent them from choking while sleeping on their backs.
Babies who sleep on their backs are much less likely to die of SIDS than babies who sleep on their sides or stomachs.

Place your baby on the back for all sleep times for naps & at bedtime.
2. Use a firm sleep surface, such as a mattress in a safety-approved crib or bassinet, covered only by a fitted sheet. Some parents might feel like they should place their baby on a soft surface, such as memory foam, to help him or her to be more comfortable while sleeping. However, soft surfaces can increase the risk of sleep-related death. A firm sleep surface helps reduce the risk of SIDS and suffocation.
3. Have the baby share your room, not your bed. Your baby should not sleep in an adult bed, on a couch, or on a chair alone, with you, or with anyone else. Some parents may feel like they should share their bed with their baby to help them feel more connected. However, accidental suffocation, strangulation, and wedging (for example, being stuck between two objects such as a mattress and a wall) can happen when a baby is sleeping in an adult bed or other unsafe sleep surfaces. Room sharing is much safer than bed sharing and may decrease the risk of SIDS by as much as 50%.
4. Keep soft objects, such as pillows and loose bedding out of your baby’s sleep area. Some parents may feel they should add soft objects to their baby’s crib to help keep their baby warm and comfortable while sleeping. However, soft objects and loose bedding, like stuffed toys, sheets, comforters, and blankets, can increase the risk of suffocation and other sleep-related deaths. If you’re worried about your baby getting cold during sleep, you can dress her or him in sleep clothing (like a wearable blanket) to keep your baby warm.
5. Do not allow smoking around your baby. Smoke in the baby’s surroundings is a major risk factor for SIDS. Quitting smoking can be hard, but it is one of the best ways parents and caregivers can protect their health and their baby’s health. For help in quitting, call the quitline at 1-800-QUIT-NOW (1-800-784-8669) or visit smokefree.gov.
6. Breastfeed as Long as You Can
Breastfeeding your baby can lower the risk of SIDS by as much as 50%, though experts aren’t sure why. Some think breast milk may protect babies from infections that raise their SIDS risk. Do not drink alcohol if you breastfeed, because that raises your baby’s risk of SIDS. In addition, the simple touch is helpful. Skin-to-skin contact is important for your baby’s development.
7. Immunize Your Baby
Evidence shows babies who’ve been immunized in accordance with recommendations from the American Academy of Pediatrics and the CDC have a 50% reduced risk of SIDS compared with babies who aren’t fully immunized.
8. Consider Using a Pacifier to Put Baby to Sleep
Putting your baby to sleep with a pacifier may also help prevent SIDS, though researchers aren’t sure why. There are a few tips to follow when using a pacifier:
- If you’re breastfeeding, wait until your baby is breastfeeding regularly (at least 1 month old) before starting to use a pacifier. Introducing a pacifier too soon can lead to nipple confusion and cause your baby to prefer the pacifier’s nipple over your own.
- Don’t force your baby to take the pacifier if he doesn’t want it.
- Put the pacifier in your baby’s mouth when you put him down to sleep, but don’t put it back in his mouth after he falls asleep.
- Keep the pacifier clean, and buy a new one if the nipple is damaged.
- Don’t coat the pacifier with honey, alcohol, or any other substance.
9. Keep Your Baby From Overheating
Because overheating may raise a baby’s risk of SIDS, dress your infant in light, comfortable clothes for sleeping, and keep the room temperature at a level that’s comfortable for an adult.
If you’re worried about your baby staying warm, dress him in a “onesie,” pajamas that cover arms, legs, hands, and feet, or place him in a “sleep sack” (a wearable blanket). However, don’t use a regular blanket — your baby can get tangled in it or pull the blanket over his face.
10. Steer Clear of Products That Claim to Reduce the Risk of SIDS
It’s best to avoid any product that says it can lower your baby’s risk of SIDS, because they haven’t been proven safe or effective. Cardiac monitors and electronic respirators also haven’t been proven to reduce SIDS risk, so avoid these, too.
11. Don’t Give Honey to an Infant Under 1 Year Old
Because honey can lead to botulism in very young children, never give honey to a child under 1 year old. Botulism and the bacteria that cause it may be linked to SIDS.
Remember, your baby’s health care provider is always available to answer any questions you have about SIDS, SIDS prevention, and keeping your baby warm, happy, and safe.
QUOTE FOR MONDAY:
“As a result of efforts by the Institute and other organizations, the sudden infant death rate is at an all-time low. However there are still about 4,000 sleep-related infant deaths that occur each year in the US. This research is aimed at identifying possible medical vulnerabilities that put infants at greater risk for sudden death.”
American SIDS Institute