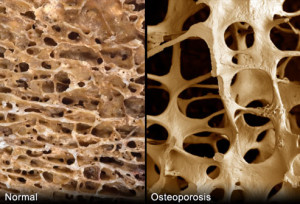

How the neck of the foramen breaks due to Osteo.
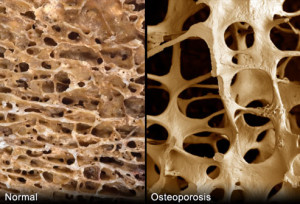
Its a progressive bone disease that is characterised by a decrease in bone mass and density and that leads to an increased risk of fracture. In osteoporosis, the bone mineral density (BMD) is reduced, bone microarchitecture deteriorates, and the amount and variety of proteins in bone are altered.
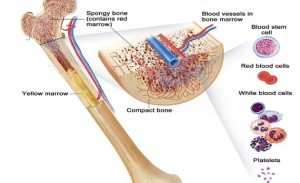
Osteoporosis causes bones to become weak and brittle —- so brittle that a fall or even mild stresses like bending over or coughing can cause a fracture. Osteoporosis-related fractures most commonly occur in the hip, wrist or spine. Bone is living tissue, which is constantly being absorbed and replaced. Osteoporosis occurs when the creation of new bone doesn’t keep up with the removal of old bone. Osteoporosis affects men and women of all races; but white and Asian women–especially after menopause–are at highest risk. Medications, healthy diet and weight bearing exercise can help prevent bone loss or strengthen already weak bones.
A weight bearing exercise is any exercise that has your legs and feet holding all of your weight. An example of this would be walking, yoga or even dancing.
The form of osteoporosis most common in women after menopause is referred to as primary type 1 or postmenopausal osteoporosis. Primary type 2 osteoporosis or senile osteoporosis occurs after age 75 and is seen in both females and males at a ratio of 2:1. Secondary osteoporosis may arise at any age and affect men and women equally. This form results from chronic predisposing medical problems or disease, or prolonged use of medications such as glucocorticoids, when the disease is called steroid- or glucocorticoid-induced osteoporosis.
The risk of osteoporosis fractures can be reduced with lifestyle changes and in those with previous osteoporosis related fractures medications. Lifestyle change includes diet, exercise, and preventing falls. The utility of calcium and vitamin D is questionable in most. Bisphosphonates are useful in those with previous fractures from osteoporosis but are of minimal benefit in those who have osteoporosis but no previous fractures. Osteoporosis is a component of the frailty syndrome.
Take the problem of Astronauts with osteoporosis:
Space travel has made it widely known that a stay outside the atmosphere – and thus outside the earth’s gravitational influence – disturbs the metabolism irreparably: the human body does not need any hard bones in zero-gravity, which leads to decalcification. A four year study of the ‘International Space Station’ showed that the bones of astronauts did not regenerate after even one year past their return to earth.
Anti-gravitational training is the key to osteoporosis if you can handle it (like jumping on a trampeline) Actual studies show that physical anti-gravitational activity helps the effected patients to regain their mobility and lessen the risk of bone fractures .
Osteoporosis in the U.S.A.
The National Osteoporosis Foundation (NOF) today released updated prevalence data estimating that a total of 54 million U.S. adults age 50 and older are affected by osteoporosis and low bone mass. Recently published online by the Journal of Bone and Mineral Research, the study, “The Recent Prevalence of Osteoporosis and Low Bone Mass in the United States Based on Bone Mineral Density at the Femoral Neck or Lumbar Spine,” includes the number of adults age 50 and over from the institutionalized and non-institutionalized population affected by osteoporosis and low bone mass and is an update to the prevalence data NOF released in 2013. Revealing that 10.2 million adults have osteoporosis and another 43.4 million have low bone mass, more than one-half of the total U.S. adult population is currently affected.
Assuming osteoporosis and low bone mass prevalence remain unchanged, the study projects that by 2020, the number of adults over age 50 with osteoporosis or low bone mass will grow from approximately 54 million to 64.4 million and by 2030, the number will increase to 71.2 million (a 29% increase from 2010); and it is anticipated that the number of fractures will grow proportionally.
“This disease causes an estimated two million broken bones each year and often results in immobility, pain, placement in a nursing home, isolation and other health problems, said Amy Porter, executive director and CEO of NOF. “Medicare (our tax dollars) pays for the cost for repair of 80 percent of broken bones that occur because of osteoporosis; these costs make osteoporosis the 10th ranked major illness among the top 5% highest cost Medicare beneficiaries (12% of all beneficiaries and 18% of high costs beneficiaries). We have to continue our efforts to eradicate this disease.”
The data is one of the first to look at the burden of osteoporosis using NOF’s criteria for diagnosing osteoporosis based on bone mineral density (BMD) at the hip or spine. Prior to 2005, the National Health and Nutrition Examination Survey (NHANES) only measured BMD at the hip. Spine BMD was added in 2005, providing the opportunity to estimate the burden of osteoporosis using BMD at either the hip or spine. The study estimates that among adults age 50 years and older, 10.2 million have osteoporosis at the femoral neck or lumbar spine and an additional 43.4 million have low bone mass at either skeletal site, placing them at increased risk for osteoporosis and broken bones.
Benefits of exercise
Women who have been physically active throughout their lives generally have stronger bones than do women who have led more sedentary lives. But it’s never too late to start exercising. For postmenopausal women, regular physical activity can:
- Increase your muscle strength
- Improve your balance
- Make you better able to carry out daily tasks and activities
- Maintain or improve your posture
- Relieve or decrease pain
- Improve your sense of well-being Before you start having osteoporosis.
- Consult your doctor before starting any exercise program for osteoporosis. You may need some tests first, including:
- Exercising if you have osteoporosis means finding the safest, most enjoyable activities for you given your overall health and amount of bone loss. There’s no one-size-fits-all prescription.
- Bone density measurement
- Fitness assessment
In the meantime, think about what kind of activities you enjoy most. If you choose an exercise you enjoy, you’re more likely to stick with it over time.