Archive | June 2018
QUOTE FOR FRIDAY:
““Thirty years ago this month, President Ronald Reagan issued a presidential proclamation designating the last week of June as “Helen Keller Deaf-Blind Awareness Week.” Every year since, the Helen Keller National Center for Deaf-Blind Youths & Adults (HKNC) commemorates the week with a national advocacy campaign in recognition of the achievements and capabilities of people who are deaf-blind.”
AHC – American Health Council
QUOTE FOR THURSDAY:
“If a child is born totally blind, how will that limitation affect her connection with those around her? The literature estimates that 75%of most people’s learning comes through vision (Smith & Cote, 1982). A deaf infant with normal vision will not have the same trouble developing early bonds with his caregivers as an infant who is blind because, as we have seen,the eyes are a main avenue for these early bonds.”
National Center on Deaf and Blindness (nationaldb.org)
QUOTE FOR TUESDAY:
“Sinusitis usually occurs after a viral upper respiratory infection or cold and includes thick, discolored nasal mucus, decreased sense of smell, and pain in one cheek or upper teeth. Headaches due to sinus disease often last days or longer and migraine headaches most commonly last hours to a day or two. Headaches due to sinus disease often last days or longer and migraine headaches most commonly last hours to a day or two.”
MAYO Clinic
QUOTE FOR MONDAY:
“Nasal sinus disease, or sinusitis, affects approximately 33 million people and accounts for more than $5.8 billion in healthcare costs annually, according to a release from Monell. Most of the time, the condition is caused by infection or allergy, which, in turn, causes sinus tissues to swell.”
NBC NEWS
It’s that time of the season again, Sinuses!
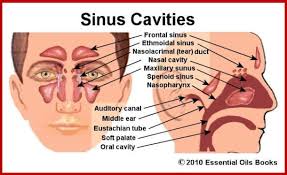
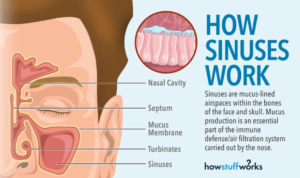
The sinus cavities include:
• The maxillary sinuses (the largest), in the cheekbones.
• The frontal sinuses, in the low-center of the forehead.
• The ethmoid sinuses, between the eyes, at the nasal bridge.
• The sphenoid sinuses, in bones behind the nasal cavity.
The sinuses are lined with soft, pink tissue called mucosa. Normally, the sinuses are empty except for a thin layer of mucus.
The inside of the nose has ridges called turbinates. Normally these structures help humidify and filter air. The nose is divided in the center by a thin wall, called the septum. Most of the sinuses drain into the nose through a small channel or drainage pathway called the middle meatus.
The purpose of the sinuses is unclear. One theory is that sinuses help humidify the air we breathe in; another is that they enhance our voices.
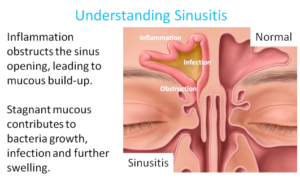
There are millions of bacteria in our noses, and most of the time, they’re harmless. Even when a few creep into the sinuses, they don’t cause trouble, as long as they keep draining into the nose along with mucus. But if sinus drainage is blocked, glands in the sinuses continue to produce mucus, and the resulting pool of backed-up mucus provides what Dr. Metson calls “the perfect culture medium.” The bacteria grow out of control, causing infection, and the immune system kicks off an inflammatory response. The result: swelling, which causes headache and facial pain; mucus buildup, which produces congestion; and an influx of white blood cells to fight the bacteria, which thickens the mucus and may tint it yellow or green. Other symptoms include loss of smell or taste, cough, bad breath, fever, toothache, and fullness in the ears.Sinus blockage can have a variety of environmental, anatomical, and genetic causes, but the main culprit is swelling of the nasal passages produced by the common cold or allergies. More serious sinusitis can result from structural problems, such as a deviated septum (a crook in the partition that separates the right from left nasal cavities) or nasal polyps (small, grapelike growths in the lining of the sinus cavity).
QUOTE FOR THE WEEKEND:
“As a person gets older, changes occur in all parts of the body, including the brain. Certain parts of the brain shrink, especially those important to learning and other complex mental activities.”
NIH National Institute on Aging
How aging affects the human brain and our thinking.
The brain controls many aspects of thinking—remembering, planning and organizing, making decisions, and much more. These cognitive abilities affect how well we do everyday tasks and whether we can live independently.
Some changes in thinking are common as people get older. For example, older adults may have:
- Increased difficulty finding words and recalling names
- More problems with multi-tasking
- Mild decreases in the ability to pay attention
Aging may also bring positive cognitive changes. People often have more knowledge and insight from a lifetime of experiences. Research shows that older adults can still:
- Learn new things
- Create new memories
- Improve vocabulary and language skills
The Older, Healthy Brain
As a person gets older, changes occur in all parts of the body, including the brain.
- Certain parts of the brain shrink, especially those important to learning and other complex mental activities.
- In certain brain regions, communication between neurons (nerve cells) can be reduced.
- Blood flow in the brain may also decrease.
- Inflammation, which occurs when the body responds to an injury or disease, may increase.
These changes in the brain can affect mental function, even in healthy older people. For example, some older adults find that they don’t do as well as younger people on complex memory or learning tests. Given enough time, though, they can do as well. There is growing evidence that the brain remains “plastic”—able to adapt to new challenges and tasks—as people age.
It is not clear why some people think well as they get older while others do not. One possible reason is “cognitive reserve,” the brain’s ability to work well even when some part of it is disrupted. People with more education seem to have more cognitive reserve than others.
Some brain changes, like those associated with Alzheimer’s disease, are NOT a normal part of aging. Talk with your healthcare provider if you are concerned.
Brain Regions
The brain is complex and has many specialized parts. For example, the two halves of the brain, called cerebral hemispheres, are responsible for intelligence.
The cerebral hemispheres have an outer layer called the cerebral cortex. This region, the brain’s “gray matter,” is where the brain processes sensory information, such as what we see and hear. The cerebral cortex also controls movement and regulates functions such as thinking, learning, and remembering.
For more information about parts of the brain, see Know Your Brain from the National Institute of Neurological Disorders and Stroke, part of the National Institutes of Health.
How Brain Cells Work
The healthy human brain contains many different types of cells. Neurons are nerve cells that process and send information throughout the brain, and from the brain to the muscles and organs of the body.
The ability of neurons to function and survive depends on three important processes:
- Communication. When a neuron receives signals from other neurons, it generates an electrical charge. This charge travels to the synapse, a tiny gap where chemicals called neurotransmitters are released and move across to another neuron.
- Metabolism. This process involves all chemical reactions that take place in a cell to support its survival and function. These reactions require oxygen and glucose, which are carried in blood flowing through the brain.
- Repair, remodeling, and regeneration. Neurons live a long time—more than 100 years in humans. As a result, they must constantly maintain and repair themselves. In addition, some brain regions continue to make new neurons.
Other types of brain cells, called glial cells, play critical roles in supporting neurons. In addition, the brain has an enormous network of blood vessels. Although the brain is only 2 percent of the body’s weight, it receives 20 percent of the body’s blood supply.
QUOTE FOR FRIDAY:
“While the heart is one of the first organs to begin development, it takes several weeks before it resembles the four-chambered structure that we all know. When the human heart first begins to form, it looks like a simple tube, much like a fish’s heart. However, rapid growth soon causes the tube to bend and twist backward, beginning the formation of the familiar shape.”
Franklin Institute
The heart is the engine of the human body.
Uncontrolled high blood pressure is of considerable concern because of what harm it can do to the HEART, BRAIN, and KIDNEYS, if it remains uncontrolled:
Heart=Angina to Heart Attack (infarction) 2- Brain=Transient Ischemia Attack (TIA) to a stroke 3- Kidneys=Reducing blood suppy to kidneys causing the kidneys to secrete RENIN into the blood. This enzyme breaks down angiotensin from the plasma protein (a powerful blood constrictor in the blood ) making the blood pressure higher. It stimulates aldosterone release in our blood stream that promotes sodium and water retention in the blood ,= increases your B/P more due to how it works.
These 3 organs with conditions are all due to obstruction of blood flow to the organs and due to the effect the high blood pressure climbs, and the heart must work or pump harder=things that happen to our engine/heart:
One, the heart muscle tissue eventually thickens and the heart becomes ENLARGED causing it not to do its job properly causing it to go in time into failure.
Two, is stress to the heart = lack of oxygen = chest pain (angina) or myocardial infarction (heart attack). When we stress the heart out=overworked, lack of oxygen to the heart tissue happens = pain as a symptom (we call it Angina that can be reversed) and if it continues it can lead to a heart attack = scarring to the heart tissue= damage done to the heart that’s not reversible. Also with constant HTN which can cause constriction of vessels in the brain this can cause the same stress but with different symptoms, the brain with uncontrolled HTN can cause lack of oxygen to the brain = headache which if not resolved can lead to a TIA (reversible) or stroke (scarring to the brain, not reversible). All of these responses are made worse by low potassium intake and high sodium intake orally (in a lot of cases these conditions could have been controlled via diet, exercise with balancing it with rest and check up with a doctor (cardiac especially).
2 – Arteriosclerosis or Atherosclerosis both = CAD (Coronary Artery Disease)
This is a common disorder, typically affecting men over age 50 and women as well but possibly earlier. People are at higher risk if they have a personal or family history of coronary artery disease (heart disease) or cerebrovascular disease (stroke), diabetes, smoking, hypertension (high blood pressure), or kidney disease involving hemodialysis. Than live healthy if you want to live longer and not get these risks or even if you do have them already than be compliant in reaching your optimal level of health with the disease. If no history and not diagnosed yet with any of these but want to prevent it live healthy, if you’re not. Arteriosclerosis is hardening of the arteries, which occurs with aging (wear and tear from also practicing bad habits that takes over years allowing this to form not just due to age; that’s why most books state it happens later in life. As opposed to adults not too many with cardiac disease young). Atherosclerosis is a form of arteriosclerosis but this is the lipid related arterial lesion, is the major disease responsible for the principle clinical complications = BLOCKAGE in the arteries. Definitely affected if already with high cholesterol and fats in the diet and of course smoking from tar build up in the vessel. Over time CAD can weaken the heart muscle also causing the heart to go into decompensation causing symptoms of chest pain=angina to even a heart attack. This may lead to heart failure, a serious condition where the heart can’t pump blood the way that it should. Even an irregular heartbeat, or arrhythmia, can also develop that if it gets worse could lead into cardiac arrest. The CDC states under CHF (congestive heart failure) “Diseases that damage your heart—including coronary heart disease, high blood pressure, and diabetes—are common causes of heart failure. Smoking; being overweight; eating foods high in fat, cholesterol, and sodium; and physical inactivity also increase your risk of developing heart failure.” Let’s wake up America with health and practicing good habits to decrease your risk of developing these diseases.
High Cholesterol levels — High cholesterol is one of the leading causes of heart attacks. Cholesterol is transported through your blood in two ways: the low density lipoprotein (LDL), which transports cholesterol to the cells that need it, and the high density lipoprotein (HDL), which is the healthy cholesterol that reduces your risk for heart attack. Having high LDL levels raises your risk of having heart disease by 20%. Losing 11-20 pounds can help you significantly reduce your cholesterol level so you prevent blockage from occurring preventing heart attack and atherosclerosis.
A sedentary lifestyle and lifetime lack of exercise seems to be major contributing factors for getting arteriosclerosis and heart-disease onset; see how they all interrelate with one causing another people.
Starting to get it? That based on how healthy you live in many cases is the determining factor of how you turn out regarding disease, but there are non-modifiable risk factors to disease (not controllable) = 1.) Age 2.) Sex (Ex. A higher amount of cases with HTN are males vs. females). 3. Race (Ex. African American have a higher count in HTN than Caucasian) 4. Heredity.
Modifiable Risk Factors (things you can change that effect diseases) = 1- weight 2- smoking 3 – living conditions 4 – diet 5 – The health & unhealthy habits you practice.
How to prevent these cardiac conditions all listed above, don’t live the type of life that’s unhealthy, at least on a regular basis (if at all occasionally live unhealthy – Ex. eating fast foods) to decrease the chances of developing these cardiac conditions that are high in America now and have been for several years. Need help and guidance in how to go about this; then you are on the right website. The answer to prevention or treatment of cardiac disease is in changing or modifying your diet, if it’s unhealthy 100% or just partially. The answer includes exercise (from just walking fast or if you like working out, even better) and if needed medication your doctor will decide that, particularly cardiac – the specialist for this area. All these changes can modify your blood lipid profile = cholesterol control, which helps increasing your heart to a better tolerance with activity, stress and simply functioning. Recommended is going to a cardiologist for people diagnosed with heart conditions or your general practitioner with any illness/disease before making changes to help guide you towards the right choices. Your doctor can help you in determining which prevention or treatment plan is best for you.
Bad Foods high in cholesterol too avoid = Fast foods, whole fat dairy products = milk/cheese/ butter/mayonnaise/bacon/processed deli meats/salad dressings/shortening.
The key is to living a healthy life overall. This consists of diet, exercise or activity and healthy habits learned and practiced routinely in your life that will help prevent or assist you in treating cardiac disease. The better we treat ourselves regarding health the higher the odds we will live a longer life. It is pretty simple. There is not just one food to eat or one type of exercise to do or one healthy habit to keep you healthy, there are choices.