“Winning feels good, but youth sports is about so much more than that, with higher stakes than any football game or soccer match.
Archive | August 2025
Why youth sports are important!
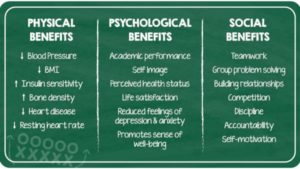
Regular physical activity benefits health in many ways, including helping build and maintain healthy bones, muscles, and joints; helping control weight and reduce fat; and preventing or delaying the development of high blood pressure (GAO, 2012). Exercise is one of the least expensive ways to stay healthy, with one study finding that exercise can prevent chronic diseases as effectively as medication (British Journal of Medicine, 2013). A comprehensive study and analysis of existing research found that leisure-time physical activity is associated with reduced risk of 13 different types of cancer, including breast, colon, liver and myeloid leukemia (National Institutes of Health, 2016).
Sports participation is a significant predictor of young adults’ participation in sports and physical fitness activities. Adolescents who play sports are eight times as likely to be active at age 24 as adolescents who do not play sports (Sports Participation as Predictors of Participation in Sports and Physical Fitness Activities in Young Adulthood, Perkins, 2004). Three in four (77%) of adults aged 30+ who play sports today played sports as school-aged children. Only 3% of adults who play sports currently did not play when they were young (Robert Wood Johnson Foundation/Harvard University/NPR, 2015).
Obesity reduction. In a 2014 study published in the American Journal of Preventive Medicine, researchers analyzed obesity prevention strategies and their ability to reduce obesity by the year 2032. They found afterschool physical activity programs would reduce obesity the most, 1.8% among children ages 6 to 12. That’s twice the projected impact as any ban on child-directed fast-food advertising. An earlier study of college students found that “motives for sport participation are more desirable than those for exercise and may facilitate improved adherence to physical activity recommendations” (Kilpatrick, Journal of American College Health, 2005).
But the obesity epidemic continues. In 2018, a study published by the American Academy of Pediatrics showed overweight and obesity rates increased in all age groups among children ages 2 to 19 (Prevalence of Obesity and Severe Obesity in U.S. Children, 1999-2016). The rates generally increased with age, with 41.5% of teens being obese by 16 to 19 years old. Of particular concern were continued racial and ethnic disparities. White and Asian children showed significantly lower rates of obesity than Hispanic and African-American children. Researchers also found a sharp increase in obesity from 2015 to 2016 compared to the previous cycle among children ages 2 to 5, especially boys. Girls 16 to 19 years old had a notable jump in overweight rates, from 36% in 2013-14 to 48% in 2015-16. Youth who have disabilities are 4.5 times less active and have obesity rates that are 38% higher than other youth (Physical Literacy in the United States: A Model, Strategic Plan, and Call to Action, 2015).
Not enough children are active. A 2018 study from Nationwide Children’s Hospital showed that just 5% of youth ages 5 to 18 reported meeting the federally recommended amount of exercise — 60 minutes per day. The study, which examined 7,822 children over three years, also found that 50 percent were insufficiently active and 5 percent reported no physical activity. Researchers recommended that pediatricians should treat exercise like a vital sign, similar to height and weight, and engage patients in conversations about how to be more physically active. A 2020 study found that 60% of American children had inadequate levels of cardiorespiratory fitness, putting them at increased risk of chronic diseases at younger ages (American Heart Association, 2020). The Aspen Institute’s Healthy Sport Index is a tool that can help parents find the best sport for their child based on health benefits and risks. The resource includes original research that found boys generate more vigorous physical activity at high school practices than girls (North Carolina State University, 2018).
EDUCATIONAL BENEFITS
From the Sport for All, Play for Life report. click to enlarge
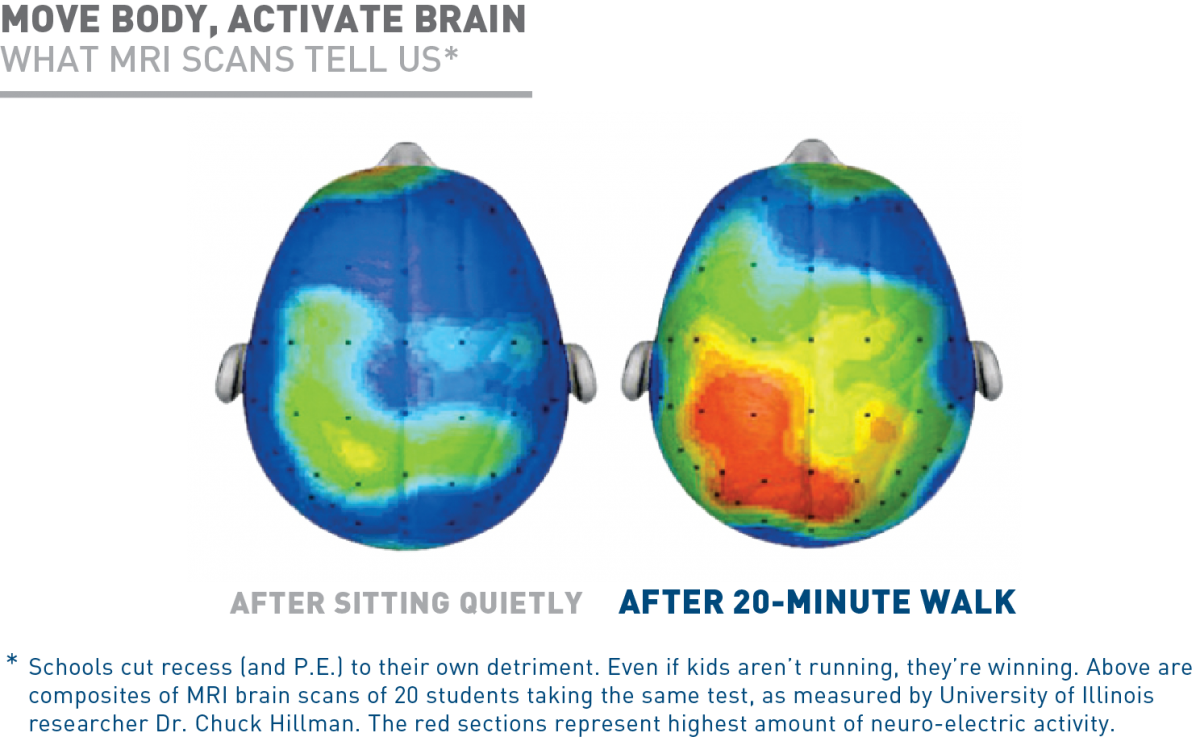
Organized sports activity helps children develop and improve cognitive skills, according to a study that tracked kids from kindergarten through fourth grade (Piche, 2014). Physical activity in general is associated with improved academic achievement, including grades and standardized test scores. Further, such activity can affect attitudes and academic behavior, including enhanced concentration, attention, and improved classroom behavior (GAO, 2012).
High school athletes are more likely than non-athletes to attend college and get degrees, and team captains and most valuable players achieve in school at even higher rates (U.S. Dept. of Education, 2005). Also, high school athletes are more likely to expect to graduate from a four-year college (73% girls, 59% boys) compared to non-athletes (67% girls, 53% boys), according to data collected for the Healthy Sport Index (Women’s Sports Foundation, 2018). A higher percentage of high school athletes also receive A/A- grades than non-athletes (Women’s Sports Foundation, 2018).
The benefits extend to the workplace. A survey of 400 female corporate executives found 94% played a sport and that 61% say sports contributed to their career success (EY Women Athletes Business Network/espnW, 2014).
PSYCHOSOCIAL BENEFITS
A correlation has been found between regular exercise and mental health among students in general as they move into the teenage years. Among students who exercised six to seven days a week, 25.1% felt sad for two weeks or more in the past 12 months, compared to 35.7% of students who reported exercising on zero to one day (Women’s Sports Foundation, 2004). Of students who exercised six to seven days, 15% reported suicidal ideation, and 6.4% reported a suicide attempt in the past year, compared to 24.6% and 10.3% of students who exercised zero to one day, respectively (Journal of American Academy of Child & Adolescent Psychiatry, 2015). A 2019 study found that children who reported no exercise were twice as likely to have mental health problems, particularly related to anxiety and depression, compared with those who met the recommendation of an hour a day, and a 2020 study suggested that the more physical activity teenagers participated in, the less likely they were to report depression as 18-year-olds (The New York Times, 2020).
Physical activity, and sports in particular, can positively affect aspects of personal development among young people, such as self-esteem, goal-setting, and leadership. However, evidence indicates that the quality of coaching is a key factor in maximizing positive effects (GAO, 2012).
Both male and female high school athletes are less likely to smoke cigarettes and suffer from loneliness and low self-esteem, when compared to non-athlete peers, according to research used for the Healthy Sport Index (Women’s Sports Foundation, 2018). High school athletes, though, are more likely to binge drink alcohol, with youth in contact sports (football, lacrosse, wrestling) showing the riskiest off-field behavior).
QUOTE FOR MONDAY:
“Empty nest syndrome refers to the distress and other complicated emotions that parents often experience when their children leave home.
Of course, people want their children to grow up and lead independent lives. However, the experience of letting go is often bittersweet or emotionally challenging. Parents may feel lonely, sad, and have some degree of grief when their children leave the nest, whether it’s to live on their own, start a college career, or pursue their own relationships. Women normally suffer more than men do, and feelings of sadness may be more pronounced among stay-at-home parents whose lives were organized around meeting the everyday needs of their children.
This empty nest syndrome that many parents of adult children experience is not a clinical disorder or diagnosis. It reflects the emotional ambivalence of a normal life transitional period.”
Psychology Today (Empty Nest Syndrome | Psychology Today)
Empty Nest Syndrome –
Empty nest syndrome is not a clinical diagnosis. Instead, empty nest syndrome is a phenomenon in which parents experience feelings of sadness and loss when the last child leaves home. Empty nest syndrome usually happens in female parents aged between 40-50. When their children have to leave home e.g. for continuing their study in the college or university, parents have to stay home alone without routine activities with their children. Although parents might actively encourage their children to become independent, the experience of letting go can be painful. Parents might find it difficult to suddenly have no children at home who need their care. Parents might miss being a part of their children’s daily lives as well as the constant companionship. These changes might develop stress, anxiety and depression. It might eventually induce suicidal thought of the parents.
With reference to Kübler-Ross, Swiss-American psychiatrist, Grieving Process consists of 5 stages:
- Denial and rejection;
- Anger and acting against what had happened;
- Bargaining for keeping the hopes;
- Depression and grief; and
- Acceptance of the loss.
If parents experience feelings of loss due to empty nest syndrome, advices that might help parents adapt to this major life change include accepting the timing, keeping in touch with children, seeking support if necessary and staying positive.
If the last child is about to leave home and parents are worried about empty nest syndrome, it is highly recommended to look for new opportunities in personal and professional life. Changing focus from taking care of children in the last 2-30 years, it is more beneficial to look after parent’s own health. Keeping busy or taking on new challenges at work or at home can help ease the sense of loss as well.
TIPS IN DEALING WITH THIS IN YOUR LIFE:
1 Time management tools can help you manage your time.
2 Space time out for a verse of the day, things you’re praying about, truths to remember, and even what to let go.
3 Make a Planner from daily to weekly to monthly in what you will be doing.
4 Like I say so many times as a RN, not to far from 40 years in this career, TAKE ONE DAY AT A TIME!
5 Remember anyone can start strong but the your goal should be “finish strong”. Example, How many times have we said we would loose weight and started strong but ended weak loosing nothing putting the white flag up and restarting later all over again and it was just a broken record finishing with no results? I have, but ending strong with starting strong is much better in results making you a more confident, stronger and happier as a person.
6 What ever your dreams are in wanting to accomplish but couldn’t with the kids at home due to busy now you can try to reach your goals you wanted to strive for. Ex. Retired now, the kids left the nest, less to do at the house now but you took a degree in art years ago, have been an artist at times in your working life but had to put it on hold since you had work elsewhere to do in paying the bills but not you can now do art work. Just make sure that they are reachable goals and not impossible to reach in art work now. So you don’t set your self up for failure. You need to approach that before starting that new life goal.
Remember everything comes to an end, some things sooner than others of course, but it does not mean life is over!
QUOTE FOR THE WEEKEND:
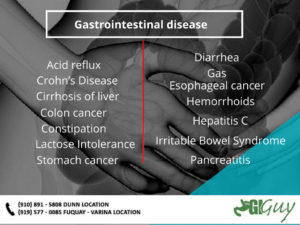
“Gastrointestinal diseases are health conditions that affect your gastrointestinal (GI) tract. Your GI tract is the path food takes through your digestive system — from your mouth to your rectum. It also includes your liver, pancreas and gallbladder. Some digestive system diseases cause problems that go away relatively fast with treatment. Others cause problems that are more serious.
GI diseases can be acute or chronic:
- An acute GI disease is one that happens suddenly and lasts a short period of time.
- A chronic GI disease can affect you for many months or years.
They can also be either functional or structural:
- A functional GI disease is when your healthcare provider can’t see any physical or structural issues when they examine your digestive tract.
- A structural GI disease is when your healthcare provider can see evidence of an issue when they examine you.
Functional gastrointestinal diseases
You’ve likely experienced several functional GI problems in your lifetime. Constipation, gas and diarrhea are examples of functional GI diseases. These types of GI diseases irritate your GI tract and lead to uncomfortable symptoms.
Some of the most common causes of functional GI problems are:
- Eating a diet low in fiber or high in processed foods
- Not getting enough exercise
- Traveling or other changes in your typical routine
- Stress and anxiety
- Holding your poop or not going as soon as you need to go
- Taking certain medicines
- Hormonal changes (like pregnancy or during menstruation)
- Food sensitivities or eating something that didn’t “agree” with you
Treatment for functional GI diseases usually involves lifestyle changes like eating more fiber-rich foods, getting more physical activity or avoiding triggers. Sometimes, functional problems go away on their own within a few days.
Structural gastrointestinal diseases
Structural GI diseases are typically more complicated. They tend to cause symptoms that last longer and don’t get better with lifestyle changes alone. Structural problems cause issues your provider can see such as inflammation or blockages. Common examples of structural GI diseases include hemorrhoids, colon polyps and inflammatory bowel disease (IBD). Causes of structural GI diseases are more widespread.”
Cleveland Clinic (Gastrointestinal Diseases: Symptoms, Treatment & Causes)
Part II Gastrointestinal Diseases – Continuation on types of GI diseases and how to prevent or deal with a GI problem!
Other perianal infections
Sometimes the skin glands near your anus become infected and need to be drained, like in this structural disease. Just behind the anus, abscesses can form that contain a small tuft of hair at the back of the pelvis (called a pilonidal cyst).
Sexually transmitted diseases that can affect the anus include anal warts, herpes, AIDS, chlamydia and gonorrhea.
Diverticular disease
The structural disease diverticulosis is the presence of small outpouchings (diverticula) in the muscular wall of your large intestine that form in weakened areas of the bowel. They usually occur in the sigmoid colon, the high-pressure area of the lower large intestine.
Diverticular disease is very common and occurs in 10% of people over age 40 and in 50% of people over age 60 in Western cultures. It is often caused by too little roughage (fiber) in the diet. Diverticulosis can sometimes develop/progress into diverticulitis
Complications of diverticular disease happen in about 10% of people with outpouchings. They include infection or inflammation (diverticulitis), bleeding and obstruction. Treatment of diverticulitis includes treating the constipation and sometimes antibiotics if really severe. Surgery is needed as last resort in those who have significant complications to remove the involved diseased segment of the colon.
Colon polyps and cancer
Each year, 130,000 Americans are diagnosed with colorectal cancer, the second most common form of cancer in the United States. Fortunately, with advances in early detection and treatment, colorectal cancer is one of the most curable forms of the disease. By using a variety of screening tests, it is possible to prevent, detect and treat the disease long before symptoms appear.
The importance of screening
Almost all colorectal cancers begin as polyps, benign (non-cancerous) growths in the tissues lining your colon and rectum. Cancer develops when these polyps grow and abnormal cells develop and start to invade surrounding tissue. Removal of polyps can prevent the development of colorectal cancer. Almost all precancerous polyps can be removed painlessly using a flexible lighted tube called a colonoscope. If not caught in the early stages, colorectal cancer can spread throughout the body. More advanced cancer requires more complicated surgical techniques.
Most early forms of colorectal cancer do not cause symptoms, which makes screening especially important. When symptoms do occur, the cancer might already be quite advanced. Symptoms include blood on or mixed in with the stool, a change in normal bowel habits, narrowing of the stool, abdominal pain, weight loss, or constant tiredness.
Most cases of colorectal cancer are detected in one of four ways:
- By screening people at average risk for colorectal cancer beginning at age 45.
- By screening people at higher risk for colorectal cancer (for example, those with a family history or a personal history of colon polyps or cancer).
- By investigating the bowel in patients with symptoms.
- A chance finding at a routine check-up.
Early detection is the best chance for a cure.
Colitis
There are several types of colitis, which are conditions that cause an inflammation of the bowel. These include:
- Infectious colitis.
- Ulcerative colitis (cause unknown).
- Crohn’s disease (cause unknown).
- Ischemic colitis (caused by not enough blood going to the colon).
- Radiation colitis (after radiotherapy).
Colitis causes diarrhea, rectal bleeding, abdominal cramps and urgency (frequent and immediate need to empty the bowels). Treatment depends on the diagnosis, which is made by colonoscopy and biopsy.
Prevention:
Can gastrointestinal diseases be prevented?
Many diseases of the colon and rectum can be prevented or minimized by maintaining a healthy lifestyle, practicing good bowel habits and getting screened for cancer.
A colonoscopy is recommended for average-risk patients at age 45. If you have a family history of colorectal cancer or polyps, a colonoscopy may be recommended at a younger age. Typically, a colonoscopy is recommended 10 years younger than the affected family member. (For example, if your brother was diagnosed with colorectal cancer or polyps at age 45, you should begin screening at age 35.)
If you have symptoms of colorectal cancer you should consult your healthcare provider right away. Common symptoms include:
- A change in normal bowel habits.
- Blood on or in the stool that is either bright or dark.
- Unusual abdominal or gas pains.
- Very narrow stool.
- A feeling that the bowel has not emptied completely after passing stool.
- Unexplained weight loss.
- Fatigue.
- Anemia (low blood count).
Other types of gastrointestinal diseases
There are many other gastrointestinal diseases. Some are discussed, but others are not covered here. Other functional and structural diseases include peptic ulcer disease, gastritis, gastroenteritis, celiac disease, Crohn’s disease, gallstones, fecal incontinence, lactose intolerance, Hirschsprung disease, abdominal adhesions, Barrett’s esophagus, appendicitis, indigestion (dyspepsia), intestinal pseudo-obstruction, pancreatitis, short bowel syndrome, Whipple’s disease, Zollinger-Ellison syndrome, malabsorption syndromes and hepatitis.
QUOTE FOR FRIDAY:
“The digestive system is a complicated and diverse part of the body. It extends from the mouth to the rectum.
- The primary function of the digestive system is to eliminate waste and assist the body in absorbing essential nutrients and minerals.
- Studies report that the gut plays a crucial role in immunity.
Every one of us has experienced digestive issues, such as stomach pain, indigestion, or discomfort, at some point in our lives for various reasons.
The medical community classifies all diseases that affect the GI tract as digestive diseases. Unfortunately, more than 85 percent of all adult Americans have some form of intestinal disorder.
The best chance for a cure is always early detection. Many GI disturbances and disorders can be avoided or reduced by leading a healthy lifestyle and undergoing regular screening as recommended.”
Medicine Net (What Are 13 Common Diseases of the Digestive System?)
Part I Gastrointestinal Diseases-What it is and types of common structural GI diseases!
What are gastrointestinal diseases?
Gastrointestinal diseases affect the gastrointestinal (GI) tract from the mouth to the anus. There are two types: functional and structural. Some examples include nausea/vomiting, food poisoning, lactose intolerance and diarrhea.
What are functional gastrointestinal diseases?
Functional diseases are those in which the GI tract looks normal when examined, but doesn’t move properly. They are the most common problems affecting the GI tract (including the colon and rectum). Constipation, irritable bowel syndrome (IBS), nausea, food poisoning, gas, bloating, GERD and diarrhea are common examples.
Many factors may upset your GI tract and its motility (ability to keep moving), including:
- Eating a diet low in fiber.
- Not getting enough exercise.
- Traveling or other changes in routine.
- Eating large amounts of dairy products.
- Stress.
- Resisting the urge to have a bowel movement, possibly because of hemorrhoids.
- Overusing anti-diarrheal medications that, over time, weaken the bowel muscle movements called motility.
- Taking antacid medicines containing calcium or aluminum.
- Taking certain medicines (especially antidepressants, iron pills and strong pain medicines such as narcotics).
- Pregnancy.
What are structural gastrointestinal diseases?
Structural gastrointestinal diseases are those where your bowel looks abnormal upon examination and also doesn’t work properly. Sometimes, the structural abnormality needs to be removed surgically. Common examples of structural GI diseases include strictures, stenosis, hemorrhoids, diverticular disease, colon polyps, colon cancer and inflammatory bowel disease.
Constipation
Constipation, which is a functional problem, makes it hard for you to have a bowel movement (or pass stools), the stools are infrequent (less than three times a week), or incomplete. Constipation is usually caused by inadequate “roughage” or fiber in your diet, or a disruption of your regular routine or diet.
Constipation causes you to strain during a bowel movement. It may cause small, hard stools and sometimes anal problems such as fissures and hemorrhoids. Constipation is rarely the sign that you have a more serious medical condition.
You can treat your constipation by:
- Increasing the amount of fiber and water to your diet.
- Exercising regularly and increasing the intensity of your exercises as tolerated.
- Moving your bowels when you have the urge (resisting the urge causes constipation).
If these treatment methods don’t work, laxatives can be added. Note that you should make sure you are up to date with your colon cancer screening. Always follow the instructions on the laxative medicine, as well as the advice of your healthcare provider.
Irritable bowel syndrome (IBS)
Irritable bowel syndrome (also called spastic colon, irritable colon, IBS, or nervous stomach) is a functional condition where your colon muscle contracts more or less often than “normal.” Certain foods, medicines and emotional stress are some factors that can trigger IBS.
Symptoms of IBS include:
- Abdominal pain and cramps.
- Excess gas.
- Bloating.
- Change in bowel habits such as harder, looser, or more urgent stools than normal.
- Alternating constipation and diarrhea.
Treatment includes:
- Avoiding excessive caffeine.
- Increasing fiber in your diet.
- Monitoring which foods trigger your IBS (and avoiding these foods).
- Minimizing stress or learning different ways to cope with stress.
- Taking medicines as prescribed by your healthcare provider.
- Avoiding dehydration, and hydrating well throughout the day.
- Getting high quality rest/sleep.
Hemorrhoids
Hemorrhoids are dilated veins in the anal canal, structural disease. They’re swollen blood vessels that line your anal opening. They are caused by chronic excess pressure from straining during a bowel movement, persistent diarrhea, or pregnancy. There are two types of hemorrhoids: internal and external.
Internal hemorrhoids
Internal hemorrhoids are blood vessels on the inside of your anal opening. When they fall down into the anus as a result of straining, they become irritated and start to bleed. Ultimately, internal hemorrhoids can fall down enough to prolapse (sink or stick) out of the anus.
Treatment includes:
- Improving bowel habits (such as avoiding constipation, not straining during bowel movements and moving your bowels when you have the urge).
- Your healthcare provider using ligating bands to eliminate the vessels.
- Your healthcare provider removing them surgically. Surgery is needed only for a small number of people with very large, painful and persistent hemorrhoids.
External hemorrhoids
External hemorrhoids are veins that lie just under the skin on the outside of the anus. Sometimes, after straining, the external hemorrhoidal veins burst and a blood clots form under the skin. This very painful condition is called a “pile.”
Treatment includes removing the clot and vein under local anesthesia and/or removing the hemorrhoid itself.
Anal fissures
Anal fissures are also a structural disease. They are splits or cracks in the lining of your anal opening. The most common cause of an anal fissure is the passage of very hard or watery stools. The crack in the anal lining exposes the underlying muscles that control the passage of stool through the anus and out of the body. An anal fissure is one of the most painful problems because the exposed muscles become irritated from exposure to stool or air, and leads to intense burning pain, bleeding, or spasm after bowel movements.
Initial treatment for anal fissures includes pain medicine, dietary fiber to reduce the occurrence of large, bulky stools and sitz baths (sitting in a few inches of warm water). If these treatments don’t relieve your pain, surgery might be needed to repair the sphincter muscle.
Perianal abscesses
Perianal abscesses, also a structural disease, can occur when the tiny anal glands that open on the inside of your anus become blocked, and the bacteria always present in these glands causes an infection. When pus develops, an abscess forms. Treatment includes draining the abscess, usually under local anesthesia in the healthcare provider’s office.
Anal fistula
An anal fistula – again, a structural disease – often follows drainage of an abscess and is an abnormal tube-like passageway from the anal canal to a hole in the skin near the opening of your anus. Body wastes traveling through your anal canal are diverted through this tiny channel and out through the skin, causing itching and irritation. Fistulas also cause drainage, pain and bleeding. They rarely heal by themselves and usually need surgery to drain the abscess and “close off” the fistula.
Check out Part II tomorrow!
QUOTE FOR THURSDAY:
“What is the home Epley maneuver?
The home Epley maneuver is a type of exercise help that helps to treat the symptoms of benign paroxysmal positional vertigo (BPPV). You can do this exercise at home.
BPPV is caused by a problem in your inner ear. Your semicircular canals are found inside your ear. They detect motion and send this information to your brain. The utricle is a nearby part of the ear. It contains calcium crystals (canaliths) that help it detect movement.
Sometimes these crystals detach from the utricle and end up inside the semicircular canals. When these crystals move inside the canals, they may send incorrect signals to your brain about your position. This can make you feel like the world is spinning. This is called vertigo.
Dr. John Epley designed a series of movements to dislodge the crystals from the semicircular canals. These movements bring the crystals back to the utricle, where they belong. This treats the symptoms of vertigo.
The original Epley maneuver was designed to be done with a healthcare provider. The home Epley maneuver is similar. These are a series of movements that you can do without help, in your own home.”
John Hopkins Medicine (Home Epley Maneuver | Johns Hopkins Medicine)
Part 3 Benign Posterior Paroxsymal Vertigo – Surgeries for it and hospital with high ratings in this area.
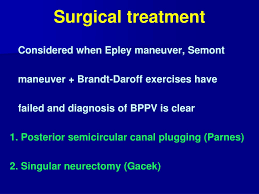
Surgical Procedures for Vestibular Dysfunction When is surgery necessary?
When medical treatment isn’t effective in controlling vertigo and other symptoms caused by vestibular system dysfunction, surgery may be considered. The type of surgery performed depends upon each individual’s diagnosis and physical condition. Surgical procedures for peripheral vestibular disorders are either corrective or destructive. The goal of corrective surgery is to repair or stabilize inner ear function. The goal of destructive surgery is to stop the production of sensory information or prevent its transmission from the inner ear to the brain. The types of surgeries used if non-invasive treatments are not successful are possibly:
Labyrinthectomy:
A labyrinthectomy is a destructive procedure used for Ménière’s disease. The balance end organs are removed so that the brain no longer receives signals from the parts of the inner ear that sense gravity and motion changes. The hearing organ (cochlea) is also sacrificed with this procedure.
Vestibular nerve section:
A vestibular nerve section is a destructive procedure used for Ménière’s disease. The vestibular branch of the vestibulo-cochlear nerve is cut in one ear to stop the flow of balance information from that ear to the brain. The brain can then compensate for the loss by using only the opposite ear to maintain balance.
Chemical labyrinthectomy:
A chemical labyrinthectomy is also known as transtympanic or intratympanic treatment or gentamicin infusion. This is a destructive procedure used for Ménière’s disease. An antibiotic called gentamicin is introduced into the middle ear and absorbed via the round window. The drug destroys the vestibular hair cells so that they cannot send signals to the brain.
Endolymphatic sac decompression:
Endolymphatic sac decompression is a stabilizing procedure sometimes used for Ménière’s disease or secondary endolymphatic hydrops to relieve endolymphatic pressure in the cochlea and vestibular system. A variety of techniques exist. One method involves allowing the sac to decompress by removing the mastoid bone surrounding it. Other methods involve inserting a shunt (a tube or strip) into the endolymphatic sac so that, theoretically, excess fluid can drain out into the mastoid cavity or other location. The effectiveness of decompression techniques in controlling vertigo remains in doubt.
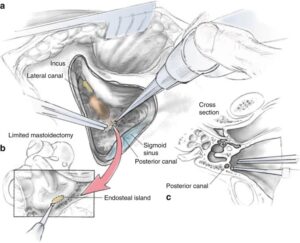
Oval or round window plugging:
If the exercises described above are ineffective in controlling symptoms, symptoms have persisted for a year or longer, and the diagnosis is very clear, a surgical procedure called “posterior canal plugging” may be recommended. Canal plugging blocks most of the posterior canal’s function without affecting the functions of the other canals or parts of the ear. This procedure poses a substantial risk to hearing — ranging from 3-20%, but is effective in about 85-90% of individuals who have had no response to any other treatment (Shaia et al, 2006; Ahmed et al, 2012). The risk of the surgery to hearing derives from inadvertent breaking into the endolymphatic compartment while attempting to open the bony labyrinth with a drill. Sensibly, canal plugging for BPPV (note the first letter stands for “benign”) is rarely undertaken these days due to the risk to hearing.
Alternatives to plugging:
Singular nerve section is the main alternative. Dr Gacek (Syracuse, New York) has written extensively about singular nerve section (Gacek et al, 1995). Interestingly, Dr. Gacek is the only surgeon who has published any results with this procedure post 1993 (Leveque et al, 2007). Singular nerve section is very difficult because it can be hard to find the nerve.
Dr. Anthony (Houston, Texas), advocates laser assisted posterior canal plugging. It seems to us that these procedures, which require unusual amounts of surgical skill, have little advantage over a conventional canal plugging procedure. Oval or round window plugging is a stabilizing procedure sometimes used for repair of perilymph fistulas. Openings in the oval and/or round windows are patched with tissue taken from the external ear or from behind the ear so that perilymph fluid does not leak through the fistulas.
Pneumatic equalization (PE) tubes:
Pneumatic equalization (PE) is a stabilizing procedure sometimes used for treating perilymph fistulas. A tube is inserted through the tympanic membrane (eardrum) with one end in the ear canal and the other in the middle ear, to equalize the air pressure on the two sides of the eardrum.
Canal partitioning (canal plugging):
Canal partitioning is a stabilizing procedure sometimes used for treating BPPV or superior semicircular canal dehiscence. The problematic semicircular canal is partitioned or plugged with small bone chips and human fibrinogen glue to stop the movement of endolymph and foreign particles within the canal so that it no longer sends false signals to the brain.
Microvascular decompression:
Microvascular decompression is performed to relieve abnormal pressure of the vascular loop (blood vessel) on the vestibulo-cochlear nerve.
Stapedectomy:
Stapedectomy is a stabilizing procedure sometimes used for otosclerosis. It is accomplished by replacing the stapes bone with a prosthesis.
Acoustic neuroma (vestibular schwannoma):
This procedure involves the removal of a noncancerous tumor that grows from the tissue of the vestibular branch of the vestibulo-cochlear nerve.
Cholesteatoma removal:
This procedure involves the removal of a skin growth that starts in the middle ear and that can secrete enzymes that destroy bone and surrounding structures.
Ultrasound surgery:
Ultrasound is applied to the ear to destroy the balance end organs so that the brain no longer receives signals from the parts of the ear that sense gravity and motion changes. Cochlear dialysis Cochlear dialysis is a stabilizing procedure sometimes used to promote movement of excess fluid out of the inner ear by filling the scala tympani with a chemical solution.
Thanks to NYU Medical Hospital in Manhattan, NY you can Click here to download the “Surgery for Peripheral Vestibular Disorders” publication. – See more at: http://vestibular.org/understanding-vestibular-disorders/treatment/vestibular-surgery#sthash.GDeNWxjl.dpuf.
If you have this problem and need a great hospital than let us look at the ranking of hospitals:
Of all 180 hospitals in the New York, New York metropolitan area, the 53 listed below are the top-ranking. This metro area, also called NYC, includes Long Island, Westchester County, and northern New Jersey. I know if I had a problem that I could not get rid of immediately with a antibiotic simple cure I would next want to go to the best if my county’s hospital couldn’t remove the problem completely. So here through “US News and World Report” via the internet they show the following information on the best hospitals in NYC and Northern NJ: (Look below or to the next page)
These are their rankings on Columbia Presbyterian and NYU, NATIONALLY, in the following categories:
Starting with the best is Columbia Presbyterian in NY, for those in NY, as your #1 choice:
Adult Specialties
This hospital was among 144 facilities—roughly 3 percent of the 4,743 analyzed for the latest Best Hospitals rankings—to be ranked in even one of the 16 specialties 2024.
COLUMBIA PRESBYTERIAN RATINGS:
| Nationally Ranked |
|
| High-Performing |
NYU HOSPITAL RATINGS:
- #50 in Cancer
- #11 in Cardiology & Heart Surgery
- #22 in Diabetes & Endocrinology
- #21 in Ear, Nose & Throat
- #26 in Gastroenterology & GI Surgery
- #8 in Geriatrics
- #38 in Nephrology
- #8 in Neurology & Neurosurgery************************ Impressive for neuro surgery of the ear.
- #4 in Orthopedics
- #33 in Pulmonology
- #9 in Rehabilitation
- #6 in Rheumatology
- #12 in Urology
Gynecology
| Rank in This Specialty | #NA |
| Overall Score in This Specialty | 66.8 / 100 |
For further checking of hospitals go to http://health.usnews.com/best-hospitals/area/ny/new-york-presbyterian-university-hospital-of-columbia-and-cornell-6210024 since hospitals do change yearly in their scores and this is the most recent.