
Now don’t get me wrong oxygen is an element that is a must for most creatures that live in the world both now and since it began but there is dangers to any element especially if mixed with some other element causing a negative result in the end. So you wonder how oxygenation can have pros and cons and why oxygen would ever have dangers to it, well let’s take a deeper look.
Oxygenation may refer to:
Oxygen saturation (medicine), the process by which concentrations of oxygen increase within a tissue
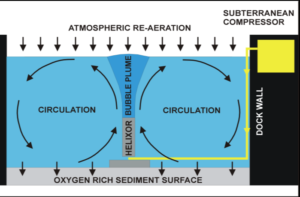
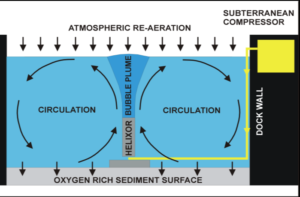
Oxygenation (environmental), a measurement of dissolved oxygen concentration in soil or water
–Great Oxygenation Event, an ancient event that led to the rise of oxygen within our atmosphere
–Water oxygenation, the process of increasing the oxygen saturation of the water
–Dioxygen complex, the chemical details of how metals bind oxygen
Of course, oxygen has its good points. Besides being necessary for respiration and the reliable combustion engine, it can be liquefied and used as rocket fuel. Oxygen is also widely used in the world of medicine as a means to imbue the body with a greater amount of the needed gas. But recent studies indicate that administering oxygen might be doing less good than hoped—and in fact be causing harm. No one is immune to the dangers of oxygen, but the people who might most suffer the ill effects are infants newly introduced to breathing, and those who are clinically deceased.
Oxygen regarding the medical view:
There are a variety of injuries and ailments for which modern medicine dictates oxygen therapy. Look at the medical aspect, the common wisdom is that by filling the lungs with pure O2, one is pushing more of the vital gas into the blood, and thus to organs that are weakened and in need of support. It has also long been known that even at partial pressures, pure oxygen can be toxic—a fact with which scuba divers and astronauts are intimately familiar. Recent studies have indicated that the human body responds to pure oxygen, even at normal pressures, in a negative way.
When pure O2 is introduced to the lungs, autonomic reflex increases respiration. The increased rate of breathing means that a much larger load of carbon dioxide is released from the body, which causes the blood vessels to constrict. Despite the increased amount of available oxygen in the lungs, the circulatory system is hampered, and cannot deliver precious O2 as well as it could when breathing normal atmosphere.
Ronald Harper, a neurobiology professor at UCLA, conducted observations on a group of healthy teenagers breathing various gas mixes using functional magnetic resonance imaging (fMRI). His findings showed that in some subjects the pure O2 caused the brain to go clinically bonkers. Brain structures such as the hippocampus, the insula, and the cingulate cortex all displayed an adverse reaction; they in turn spurred the hypothalamus, the body’s main regulatory gland, into a fervor. The hypothalamus regulates a myriad of things, including heart rate, body temperature, and is the master of a variety of other glands. The introduction of pure oxygen prompts the hypothalamus to flood the body with a cocktail of hormones and neurotransmitters which serve to hamper heart rate, and further reduce the circulatory system’s effectiveness. But Harper also found that by adding a mere 5% CO2, all the detrimental effects found in pure oxygen are negated.
There are circumstances, however, where even the proper mix of gases would prove inadequate. Modern medicine has long taught that after respiration stops, the brain can only survive for six to seven minutes without oxygen before its cells begin to die in droves. In order to combat this, standard procedure has been to aggressively attempted to restore breathing and heartbeat immediately upon cessation, CPR. The base premise on which this protocol is designed may be in error but only if continuing longer than the AHA guides us to do CPR. For there is more than just to lack of oxygen in patients who die having CPR done to them for death (Ex Exacerbation of a disease, multi – organ failure, years of CHF, etc… Even thought lack of 02 is part of the reason for the death in the end. There was a cause for it happening and leading to lack of 02 is the prime entity to death of all diseases leading up to this in a human.).
Upon examining heart cells and neurons deprived of oxygen under a microscope, Dr Lance Becker of the University of Pennsylvania found there was no indication that the cells were dying after five or six minutes. In fact, they seemed to endure the state for up to an hour without adverse affect. Given this unexpected observation, the researchers were forced to investigate why human resuscitation becomes impossible after only a few minutes of clinical death. The answer they uncovered was that the body’s cells were not dying of oxygen starvation; they were expiring due to Reperfusion—the sudden reintroduction of oxygen to a dormant cell = Programmed cell death! The cells reintroducing oxygen back into the cell from outside the cell in the bloodstream caused the destruction of the red blood cells, the RBCs carry oxygen to all our tissues sites. You would think that would save the cells in sending more oxygen out to the tissues but like we’re told from childhood too much of almost anything can hurt or kill you (Ex. Food/work/stress…)
Take a patient with severe emphysema they do get oxygen in their body but the problem is that oxygen gets air spaced elsewhere rather than all the 02 breathed in going in the red blood cells at the lungs exchange for 02 at the bottom of the lungs with CO2 (carbon dioxide) sent from the cells to the lungs to leave the body. Than the cells go off throughout the bloodstream having our tissues utilize from the red blood cells the oxygen it needs (a transfer of 02 to our tissues). Upon return of the red blood cells that took the CO2 from the tissues to keep the tissues more oxygenated, so they can do their function as an organ. Oxygen deprivation to a severe state is Oxygen Starvation to our bodies leading to death, if not reversed. Also, with the severe COPD emphysema pt their body adjusts to having high C02 levels compared to a person without emphysema. A normal person’s brain functions to sending messages out to cause us to breath when our 02 level is low but to a severe emphysema pt the low C02 levels causes their brain to send out messages to breath, so if you give an emphysema pt over 2L of 02 for several hours if will turn the brain off and the pt deceases (except when a emphysema pt is in respiratory distress, example due to cardiac arrest, since it is needed and temporary support of higher oxygen levels than when stable and out of respiratory distress their at 2L of 02 again).
Inside the cells, the culprit seems to be in the mitochondria, which is the cell’s power plant where sugar and oxygen are converted to usable energy. Mitochondria are also responsible for apoptosis—the organized, controlled self-destruction of a cell. Normally apoptosis occurs in situations such as the cell being damaged beyond repair, infected by a virus, an attempt to prevent cancer, or aiding in initial tissue development. The process effectively kills and dismantles the cell allowing the body’s usual waste management functions to carry the cell’s remains away. For reasons not entirely clear, reperfusion triggers apoptosis—the oxygen intended to save the cell actually causes cellular suicide.
Armed with this new information about how cells react to oxygen, it is clear that current emergency care is not altogether ideal, and new protocols are under investigation. Dr Becker proposes that induced hypothermia may slow cell degradation, and if a means can be found to safely reintroduce oxygen to tissues, a clinically dead person—who still has trillions of living cells—could be resuscitated after being an hour dead.
This glorious future is still on the horizon, but to imagine the practical application leads one to ponder the multitude of accidents and injuries that are currently fatal, but will one day be treatable. Emergency Medical Personnel could arrive on the scene, and inject the patient with a slurry of ice and salt that lowers the body temperature to about 92° F. In a hypothermic state, the patient is hauled to the hospital, where instead of frantically trying to restart the heart, doctors patch up the problem, prevent apoptosis , and then restart the heart. Though it won’t save everyone, these findings may lead to a future where a person made up of perfectly good human cells is not written off as dead merely because their heart has stopped beating. The miracle of modern medicine, it seems, is on the cusp of determining the true distinction between dead and mostly dead.