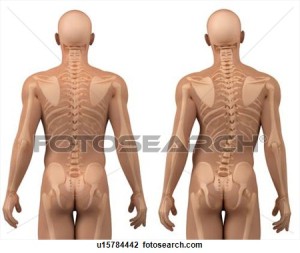
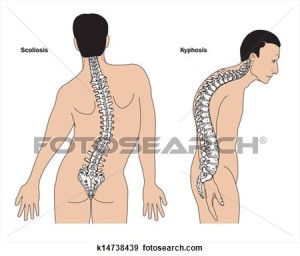
Scoliosis is a problem with the spine where the spine is curved instead of straight, with the upper back being rounded and the lower back having a “swayback,” or inner curved problem, reports WebMD.
According to the Scoliosis Research Society, 85 percent of all scoliosis causes are idiopathic, meaning the cause is unknown. The remaining causes of scoliosis include birth defects, such as vertebrae that form abnormally before birth, and certain disorders such as cerebral palsy, Marfan’s syndrome, muscular dystrophy and Down syndrome. Infections and spinal fractures can also cause scoliosis.curvature of the spine during surgical correction of this condition. Screws and rods are placed in order to stabilize and straighten the spine.
What You Should Know About Adult Scoliosis
Scoliosis is defined as a curve of the spine of 10 degrees. Adult scoliosis is broadly defined as a curve in your spine of 10 degrees or greater in a person 18 years of age or older. Adult scoliosis is separated into 2 common categories:
- Adult Idiopathic Scoliosis patients have had scoliosis since childhood or as a teenager and have grown into adulthood. We do not yet know the cause of idiopathic scoliosis, but there is a lot of genetic work going on in an attempt to answer this question.
- Adult “De Novo” or Degenerative Scoliosis develops in adulthood. Degenerative scoliosis develops as a result of disc degeneration. As the disc degenerates, it loses height. If one side of the disc degenerates more rapidly than the other, the disc begins to tilt. As it tilts, more pressure is placed on one side of your spine and gravity tends to cause the spine to bend and curve. The more discs that degenerate, the more the spine begins to curve.
Scoliosis is more common in girls than in boys, and the diagnosis is usually made after a child reaches 10 years of age. A doctor performs a physical examination and may take X-rays to definitively diagnose the disease. An X-ray tells if there is any growth left in the growth plates of the femur or humerus, and scoliosis can become worse if the patient has more growing to do, states MedicineNet. Serial X-rays are performed to track the changes of the spinal curve, which helps determine the best course of treatment.
Types of idiopathic scoliosis are categorized by both age at which the curve is detected and by the type and location of the curve.
When grouped by age, scoliosis usually is categorized into three age groups:
- Infantile scoliosis: from birth to 3 years old
- Juvenile scoliosis: from 3 to 9 years old
- Adolescent scoliosis: from 10 to 18 years old
This last category of scoliosis, adolescent scoliosis, occurs in children age 10 to 18 years old, and comprises approximately 80% of all cases of idiopathic scoliosis. This age range is when rapid growth typically occurs, which is why the detection of a curve at this stage should be monitored closely for progression as the child’s skeleton develops.
Terms Used to Describe Spinal Curvature
Scoliosis curves are often described based on the direction and location of the curve. Physicians have several detailed systems to classify specific curves, but here are some common terms used to describe scoliosis:
Terms that describe the direction of the curve:
- Dextroscoliosis describes a spinal curve to the right (“dextro” = right). Usually occurring in the thoracic spine, this is the most common type of curve. It can occur on its own (forming a “C” shape) or with another curve bending the opposite way in the lower spine (forming an “S”).
Severe scoliosis can lead to heart and lung problems if not treated, as the ribs press against the chest, making breathing more difficult, states Mayo Clinic. Adults who had scoliosis as a child may experience more back pain throughout their lives as compared to people without scoliosis.
Symptoms of scoliosis include an uneven waist, uneven shoulders, disjointed hip and a protruding shoulder blade, according to Mayo Clinic. The spine also curves or twists in acute cases, and the disease can cause one side of the ribs to protrude more than the other. Severe cases also induce labored breathing and back pain.
Diagnosis
Scoliosis can be recognized and diagnosed with a clinical exam, but xrays are necessary to fully evaluate the magnitude and type of scoliosis present. For a proper scoliosis evaluation, full length, whole spine xrays need to be performed. An MRI may also be recommended if there are symptoms of leg pain that may be associated with stenosis or if there is concern about possible spinal cord compression or abnormalities.
Treatment
The treatment of adult scoliosis is very individualized and based on the specific symptoms and age of the patient. Many patients have scoliosis and have very minor symptoms and live with it without treatment. Patients with predominant symptoms of back pain would typically be treated with physical therapy. Patients with back pain and leg pain may receive some benefit from injection treatment to help relieve the leg pain. If lumbar stenosis (narrowing of the spinal canal) is present and is unresponsive to non-surgical treatment, then a decompression( removal of bone and ligaments pressing on the nerves) may be recommended. If the scoliosis is greater than 30 degrees, a fusion procedure will most likely be recommended along with the decompression. The fusion is recommended to prevent the curve from progressing when the spine is destabilized by the bone removal that is necessary to decompress the nerves. Fusions are usually accompanied with metal rod and screw placement into the spine to help correct and stabilize the scoliosis and help the bone heal or fuse together. The length of the fusion, or the number of spine levels included, depends on the type of scoliosis and the area of the spine involved. The goal of adult scoliosis surgery is to first remove pressure on the nerves, and second to keep the scoliosis from progressing further.