More males than females are born in America each year. Still regarding health to both genders through research and just living the experience of being an RN over a quarter of a century in numerous fields (primarily of adults to geriatrics) it shows women are more healthier than men (even starting from infancy).
Out of the 15 leading causes of death, men lead women in all of them except Alzheimer’s disease, which many men don’t live long enough to develop in many cases. Although the gender gap is closing, men still die five years earlier than their wives, on average.
Through WebMD experts have told them the reason for this is that they are partly biological, and men’s approach to their health plays a role too, of course. “Men put their health last,” says Demetrius Porche, DNS, RN, editor in chief of the American Journal of Men’s Health. “Most men’s thinking is, if they can live up to their roles in society, then they’re health.” Not always the case especially when age keeps creeping up on a male with his priorities of life changing with new love or even peeps that come on board in a man’s lifetime. In most cases living healthy normally happens when are age is younger but then due to work to families to expectations leaves little room for healthier habits in the week but even 30 minutes a day could make a tremendous change to all systems of the human body preventing certain diseases/illnesses, especially those due to poor diet, eating habits and overall health habits (Ex. as simple as getting 8 hours for sleep a day).
Men go to the doctor less than women and are more likely to have a serious condition when they do go, research shows. “As long as they’re working and feeling productive, most men aren’t considering the risks to their health,” says Porche. Like a lot of men say “I don’t have to time to think about it.”. But even if you’re feeling healthy, a little planning can help you stay that way. One is through preventions measures before secondary have to start, meaning ending line your now with a disease or illness, that may have been prevented completely if you lived a healthier life. One way of preventing disease and illness is good eating or diet, with balancing out the 4 food groups (to get all nutrients from minerals to vitamins to enzymes to proteins and more). The top threats to men’s health aren’t secrets: they are commonly known and often preventable.
WebMD consulted the experts that came up with for you this list of the top health threats to men, and how to avoid them.
— “Heart disease and stroke are the first and second leading causes of death worldwide, in both men and women,” says Darwin Labarthe, MD, MPH, PhD, director of the Division for Heart Disease and Stroke Prevention at the CDC. “It’s a huge global public health problem, and in the U.S. we have some of the highest rates.” In cardiovascular disease, cholesterol plaques gradually block the arteries in the heart and brain. If a plaque becomes unstable, a blood clot forms, blocking the artery and causing a heart attack or stroke.
One in five men and women will die from cardiovascular disease, according to Labarthe. For unclear reasons, though, men’s arteries develop atherosclerosis earlier than women’s. “Men’s average age for death from cardiovascular disease is under 65,” he says; women catch up about six years later.
Even in adolescence, girls’ arteries look healthier than boys’. Experts believe women’s naturally higher levels of good cholesterol (HDL) are partly responsible. Men have to work harder to reduce their risk for heart disease and stroke. How do you go about this? Take a guess. Yes, again through your diet, eating, the 4 food groups in your diet, activity or exercise (at least 30 minutes a day or 1 hour every other day) and practicing daily good health habits.
—Lung cancer is a terrible disease: ugly, aggressive, and almost always metastatic (spreads somewhere in the body). Lung cancer spreads early, usually before it grows large enough to cause symptoms or even show up on an X-ray. By the time it’s found, lung cancer is often advanced and difficult to cure. Less than half of men are alive a year later. So … are you still SMOKING?
Tobacco smoke causes 90% of all lung cancers. Thanks to falling smoking rates in the U.S., fewer men than ever are dying of lung cancer. But lung cancer is still the leading cancer killer in men: Again due to many still practicing poor habits which could have prevented many of the lung cancer cases. Anyone who QUITS smoking at any age reduces the risk for lung cancer. Few preventive measures are as effective as stopping smoking and nothing is as challenging, like any addiction (whether mental or physical)
–Prostate Cancer: A Leading Cancer for Men
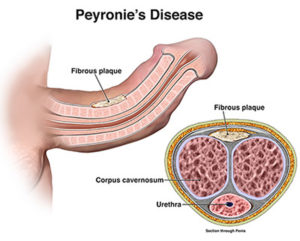
This is one health problem men can lay full claim to — after all, women don’t have prostates. A walnut-sized gland behind the penis that secretes fluids important for ejaculation, the prostate is prone to problems as men age.
Prostate cancer is the most common cancer in men other than skin cancer. Close to 200,000 men will develop prostate cancer this year in the U.S.
But while one in six men will be diagnosed with prostate cancer in his lifetime, only one in 35 will die from it. “Many prostate cancers are slow-growing and unlikely to spread, while others are aggressive,” says Djenaba Joseph, MD, medical officer for cancer prevention at the CDC. “The problem is, we don’t have effective tests for identifying which cancers are more dangerous.”
Screening for prostate cancer requires a digital rectal exam (the infamous gloved finger) and a blood test for prostate specific antigen (PSA).
But in fact, “Screening has never definitively been shown to reduce the chances of dying from prostate cancer,” according to Joseph. That’s because screening finds many cancers that would never be fatal, even if undetected. Testing then leads to aggressive treatment of relatively harmless cancers, which causes problems like impotence and incontinence.
Should you get screened for prostate cancer? Some experts say yes, but “the best solution is to see your doctor regularly and talk about your overall risk,” says Joseph. “All men should understand the risks and benefits of each approach, whichever you choose.”
–Depression and Suicide: Men Are at Risk
Depression isn’t just a bad mood, a rough patch, or the blues. It’s an emotional disturbance that affects your whole body and overall health. In effect, depression proves the mind-body connection. Brain chemicals and stress hormones are out of balance. Sleep, appetite, and energy level are disturbed. Research even suggests men with depression are more likely to develop heart disease.
The results can be tragic. Women attempt suicide more often, but men are more successful at completing it. Suicide is the eighth leading cause of death among all men; for young men it’s higher.
–Diabetes: The Silent Health Threat for Men
Diabetes usually begins silently, without symptoms. Over years, blood sugar levels creep higher, eventually spilling into the urine. The resulting frequent urination and thirst are what finally bring many men to the doctor.
The high sugar of diabetes is anything but sweet. Excess glucose acts like a slow poison on blood vessels and nerves everywhere in the body. Heart attacks, strokes, blindness, kidney failure, and amputations are the fallout for thousands of men.
Boys born in 2000 have an alarming one-in-three chance of developing diabetes in their lifetimes. Overweight and obesity are likely feeding the diabetes epidemic. “The combination of diabetes and obesity may be erasing some of the reductions in heart disease risk we’ve had over the last few decades,” warns Labarthe.
Exercise, combined with a healthy diet, can prevent type 2 diabetes. Moderate weight loss — for those who are overweight — and 30 minutes a day of physical activity reduced the chance of diabetes by more than 50% in men at high risk in one major study.
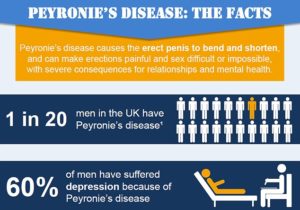
—Erectile Dysfunction: A Common Health Problem in Men
Erectile dysfunction may not be life threatening, but it’s still signals an important health problem. Two-thirds of men older than 70 and up to 39% of 40-year-old men have problems with erectile dysfunction. Men with ED report less enjoyment in life and are more likely to be depressed.
Erectile dysfunction is most often caused by atherosclerosis — the same process that causes heart attacks and strokes. In fact, having ED frequently means that blood vessels throughout the body are in less-than-perfect health. Doctors consider erectile dysfunction an early warning sign for cardiovascular disease.
You’ve probably heard more about the numerous effective treatments for ED than you ever cared to just by watching the evening news. Treatments make a fulfilling sex life possible despite ED, but they don’t cure the condition. If you have erectile dysfunction, see your doctor, and ask if more than your sex life is at risk.
So what’s the key to decreasing these diseases or illnesses in men live a healthier life so men in America can decrease the chances of developing these diseases or if with one of these diagnoses already it will surely help decrease the impact of the disease or illness compared to living an unhealthy life.
Various lifestyle factors have been associated with increasing the risk of stroke. These include lack of exercise, alcohol, diet, obesity, smoking, drug use, and stress. Guidelines endorsed by the Centers for Disease Control and Prevention and the National Institutes of Health recommend that Americans should exercise for at least 30 minutes of moderately intense physical activity on most, and preferably all, days of the week. Recent epidemiologic studies have shown a U-shaped curve for alcohol consumption and coronary heart disease mortality, with low-to-moderate alcohol consumption associated with lower overall mortality. High daily dietary intake of fat is associated with obesity and may act as an independent risk factor or may affect other stroke risk factors such as hypertension, diabetes, hyperlipidemia, and cardiac disease. Homocysteine is another important dietary component associated with stroke risk, while other dietary stroke risk factors are thought to be mediated through the daily intake of several vitamins and antioxidants. Smoking, especially current smoking, is a crucial and extremely modifiable independent determinant of stroke. Despite the obstacles to the modification of lifestyle factors, health professionals should be encouraged to continue to identify such factors and help improve our ability to prevent stroke, decrease cancers caused by smoking, decrease coronary artery disease which decreases your chance with Obesity, ED, stroke, & hypertension and more.
Learn healthy habits or healthier habits, broaden your knowledge on the 4 food groups in what is lean or leaner or leanest with each group, increase your activity 30 minutes a day and learn what a healthy diet actually is. There are many books out in the world for giving guidance like through Dr. Wayne Scott Anderson’s book “Dr. A’s habits of health” for example and even if you need to lose weight the book can show you the way to do it healthy. It’s not a diet for 3 months or even 6 months to a year but it is learning how to get to your body mass index in the ideal weight range for your height and you decide how low you want to go. There are many books out in the world that do this or even access through the internet. Just research if you need it and want it.
Join many others trying to get America healthier and in time decrease our population in diseases or illnesses primarily impacted by health habits, diet, and weight. Wouldn’t you and the future want to get better in mind and body to impact our health care system that includes our insurance and most importantly lives of citizens in the USA in how they live (which would be more active). It just takes discipline and the drive to want to stay healthy or get in a better state of heath. We can do this without changing your environment upside down and killing cattle, or living on insects but you could eat healthier foods like not fast food and lean meats with definitely vegetables, fruit and low fat foods. You can treat yourself now and than. Hope I have helped someone out there in broadening your knowledge regarding how to keep or reach a healthier life.