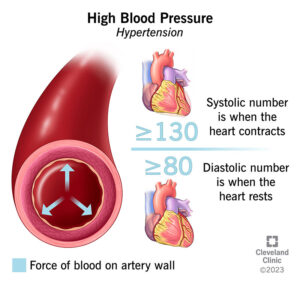
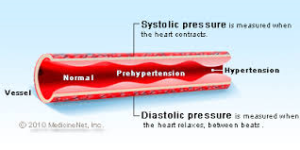
 Systolic BP is heart at work, Diastolic BP is heart at rest!
Systolic BP is heart at work, Diastolic BP is heart at rest!
High Blood Pressure – what is it?
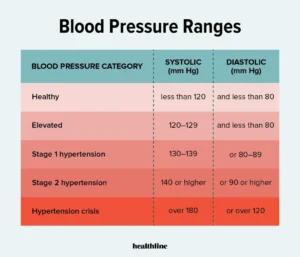
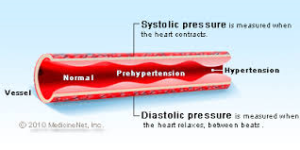
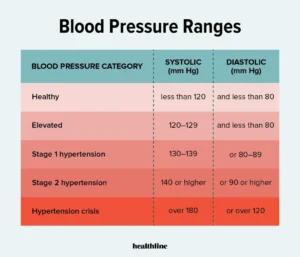
High Blood Pressure or Hypertension affects 80 million Americans and nearly half of the people in the UK between the ages of 65 and 74, and a large percentage of those between the ages of 35 and 65. One of the problems associated with high blood pressure is that you will probably not even know you have it until you happen to have your blood pressure taken during a routine physical examination. In our B/P you have 2 numbers one on the top that is called your systolic b/p that will always be higher that the bottom number b/p. What do they mean? The top number systolic B/P will be the number representing your heart pressure at work whereas the bottom number called diastolic B/P will always be lower that the top number representing the B/P at rest. Normal B/P for some is 90/50 for those who are a work out nut, in good shape, and at their normal weight level or body mass index (BMI). For others normal B/P can go has high as 120/80 or less. High B/P is over 120/80. In earlier years 122/80 was considered the norm now its not. Where do you really see problems for a high B/P? Well looking at a B/P chart this should give you some direction:
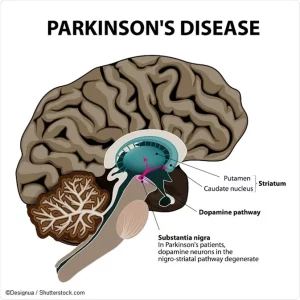
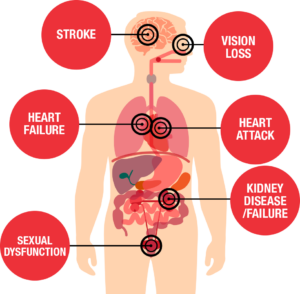
Remember in the nursing and medical field a systolic B/P of 180 these professional get concerned for stroke or a vessel somewhere about to burst (Ex. like a abdominal aneurysm which many don’t feel since its in their abdomen making room for the pouch vessel to grow making the vessel wall weaker to pop and than for many when realized its too late, take the actor John Ritter!) With a stroke it can be caused by a hemorrhagic stroke-this meaning a vessel ruptures (most commonly high B/P) or ischemic stroke a build up of a blockage or blockages of a vessel in the brain).
Upon diagnosis, you may wonder why you never saw it coming. Most people don’t. Only those with severe high blood pressure experience any warning signs at all.
These signs can include headaches, impaired vision, and black-outs.
What is blood pressure ?
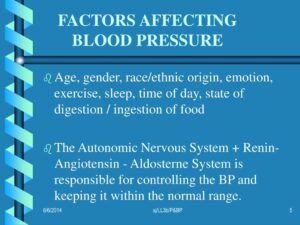
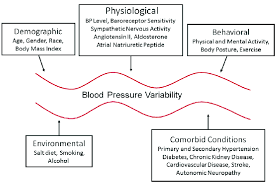
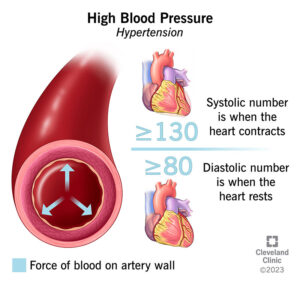
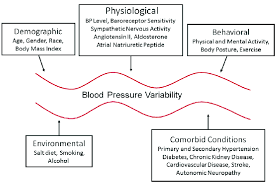
It is the measurement of the force that blood applies to the walls of the arteries as it flows through them carrying oxygen and nutrients to the body’s vital organs and systems. Naturally, our blood is under pressure as it rushes through our arteries. Even those with blood pressure in the normal range will experience an increase in their blood pressure during rigorous physical activity or during times of stress. It only becomes a problem when the blood continues to run high. This condition of blood pressure is known as hypertension or high blood pressure and in 95% of the cases, the cause of it is never known. However, we do know the factors that set a person up to develop hypertension.
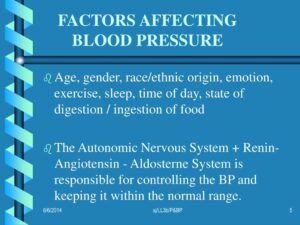
Factors influencing High Blood Pressure:
They are as follows:
NON-MODAFIABLE RISK FACTORS ARE 4:
1. HEREDITY-HIGH B/P RUNNING IN THE FAMILY
2. AGE-THE OLDER, THE HIGHER PROBABILITY YOU WILL END UP WITH B/P DEPENDING ON YOUR HEALTH AND HOW GOOD YOU TAKE CARE OF YOURSELF.
3. GENDER or SEX-MALES VS FEMALES. THE GENDER THAT BEATS THE OTHER EASILY IS MEN!
4. RACE-HIGHIER IN AFRO-AMERICAN AS OPPOSED TO WHITE.
MODAFIABLE RISK FACTORS=FACTORS YOU CAN CONTROL IN YOUR LIFESPAN:
1-Obesity=Those with a body mass index of 30 or greater.
2-Drinking more than 2 to 4 alcoholic drinks a day.
3-Smoking
4-High cholesterol
5-Diabetes
6-Ongoing Stress/Anxiety
7-Continuous use of excessive salt consumption
Possible causes of High Blood Pressure
Sometimes the cause of a person’s high blood pressure is determined, but this happens in only 5% of the cases. When a cause is found, the person is diagnosed with secondary high blood pressure [hypertension]. In most of these cases, the cause can be linked to an underlying illness such as kidney disease, adrenal gland disease, or narrowing of the aorta. Contraceptive pills, steroids, and some medications can also cause secondary high blood pressure [hypertension], though instances of this are not all that common since in most cases these can be stopped or with medications changed if a med is still needed to resolve high blood pressure.
Reviewing High Blood Pressure and the important numbers
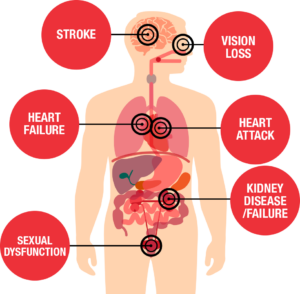
We hear the numbers, but do we really know what they mean? Since your blood pressure numbers can help you to understand your overall health status, it is important that you keep track of it. By knowing where your numbers are right now, you can head off such serious high blood pressure complications as angina, heart attacks, stroke, kidney damage, and many others that might surprise you – like eye problems and gangrene.
Hear is a review of understanding what blood pressure means and tells our medical professionals from RN’s who see the pt the most and see the vital signs with doctors being told who generally provide your blood pressure to you in terms of two numbers – a top one and a bottom one. For example, if your blood pressure is 120/80, they may say that you have a blood pressure of 120 over 80. Here is a definition again for these numbers:
The top number– this is your systolic blood pressure. It measures the force of blood in the arteries as your heart beats. The top number means the pressure is reading your heart at work. That is why this number is always highier.
The bottom number – this is your diastolic blood pressure. It is the pressure of your blood when the heart is relaxed in between the times when it is pumping. Means the pressure is reading your heart at rest. That is why the number is always lowest.
Your blood pressure requires monitoring when you have a systolic blood pressure of 140 or over and/or a diastolic blood pressure of 90 or over. Those with diabetes must maintain a lower blood pressure that those who don’t have the condition. Diabetics should maintain a blood pressure of less than 130/80. It would be ideal at 120/80 and there are some that do.
Monitors for measuring High Blood Pressure
It is wise to monitor your blood pressure at home in addition to having it taken at your doctor’s office. This will allow you to provide your doctor with readings that have been taken over time, providing a more in depth look at your personal health condition. This will help him or her to prescribe the right hypertensive medication and treatment for your specific condition.
Tips to help reduce your B/P:

The best you could do over 50 or if already diagnosed with high blood pressure than monitor it at home with automatic B/P machines or get a manual one with a stethoscope for taking your B/P measurement with your pulse for some that you take from the upper arm at home each day when you first get up. Especially have a B/P monitor is recommended in taking your B/P meds to eval how good the med is working but if on lopressor or metoprolol (commonly used antihypertensives) or any selective beta blocker which can lower your B/P and pulse. Since with metoprolol or lopressor if the b/p is 90/60 or the pulse is lower than 60 you should call the M.D. first since readings that low could bottom out your B/P and pulse with making them too low putting the pt at problems with dizziness, feeling weak to bottoming out so bad you just sleeps or better falls. So call your doctor immediately before taking the med. Always take the B/P from the upper arm above the elbow unless your M.D tells you otherwise. You’ll also want to make sure that the blood pressure monitor you are considering has been proven in clinical trials. Trusted name brands include those made by Omron, LifeSource, Mark of Fitness, Micro Life, and A and D Instruments. There are other brands available – the important thing is to do your research.
Always check with you cardiologist preferred or your general practitioner before making any changes in your lifestyle in anyway for safety.
Updated 5/07/24
 Systolic BP is heart at work, Diastolic BP is heart at rest!
Systolic BP is heart at work, Diastolic BP is heart at rest!