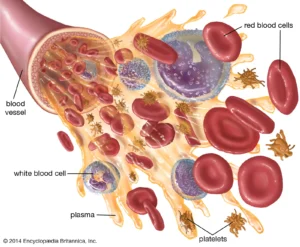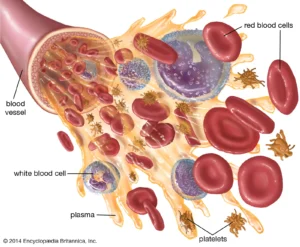
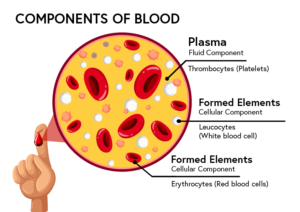
Recall that blood is a connective tissue. Like all connective tissues, it is made up of cellular elements and an extracellular matrix. The cellular elements—referred to as the formed elements—include red blood cells (RBCs), white blood cells (WBCs), and cell fragments called platelets. The extracellular matrix, called plasma, makes blood unique among connective tissues because it is fluid.
Your blood carries oxygen and nutrients to all of the cells in your body. Blood cells also fight infection and control bleeding.
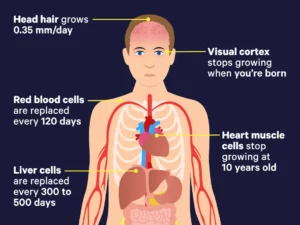
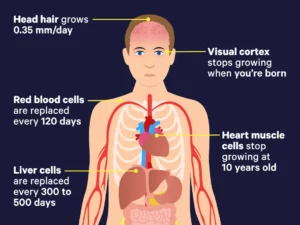
Most blood cells are made in your bone marrow. They are constantly being made and replaced. How long a blood cell lasts before being replaced is called its lifespan.
Blood is viscous, with a viscosity approximately five times greater than water. Viscosity is a measure of a fluid’s thickness or resistance to flow, and is influenced by the presence of the plasma proteins and formed elements within the blood. The viscosity of blood has a dramatic impact on blood pressure and flow. Consider the difference in flow between water and honey. The more viscous honey would demonstrate a greater resistance to flow than the less viscous water. The same principle applies to blood. Blood viscosity is inversely proportional to hydration; the more hydrated you are, the less viscous your blood becomes. In severely dehydrated individuals, blood can become excessively viscous sometimes resulting in infarction or other cardiovascular events.
The normal temperature of blood is slightly higher than normal body temperature—about 38 °C (or 100.4 °F), compared to 37 °C (or 98.6 °F) for an internal body temperature reading. Although the surface of a blood vessel is relatively smooth, blood experiences friction and resistance to its flow. This produces heat, accounting for the slightly higher temperature of blood.
The pH of blood averages about 7.4; however, it can range from 7.35 to 7.45 in a healthy person. Blood is therefore somewhat more basic (alkaline) on a chemical scale than pure water, which has a pH of 7.0. Blood contains numerous buffers that help to regulate pH.
Blood constitutes approximately 8 percent of adult body weight. Adult males typically average about 5-6 liters of blood, and females average 4–5 liters.
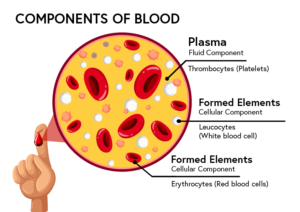
Your blood is made up of 4 parts: red blood cells, white blood cells, platelets, and plasma.
This information explains the different parts of your blood and their functions.
Your blood carries oxygen and nutrients to all of the cells in your body. Blood cells also fight infection and control bleeding.
Most blood cells are made in your bone marrow. They are constantly being made and replaced. How long a blood cell lasts before being replaced is called its lifespan. This is why for example in cancers a bone marrow aspiration commonly used in checking for blood or other cancers or bone marrow transplant used as a treatment for giving healthy hematopoietic stem cells into the diseased pt’s bone marrow to replace diseased blood cells and stimulate the production of healthy blood cells, effectively slowing down or stopping the cancer’s progression if the pt is a candidate.
Your blood is made up these 4 types of cells, lets review:
Parts of Your Blood
1-Red blood cells (erythrocytes)
Red blood cells carry oxygen from your lungs to your tissues. They also bring carbon dioxide back to your lungs.
Red blood cells make up almost half of your blood. The lifespan of a red blood cell is around 120 days.
2-White blood cells (leukocytes)
White blood cells fight infection and are an important part of your immune system. They make up a very small part of your total blood (less than 1%).
There are 3 types of white blood cells: I granulocytes, II monocytes, & III lymphocytes. Each type has an important role.
- I There are 3 types of granulocytes: A.Neutrophils help fight bacterial and fungal infections. B. Basophils are part of your body’s immune response/responses to allergens. Basophils are implicated in multiple human diseases including autoimmune disorders, inflammatory disorders, cancer and allergies and asthma. However, the contributions of basophils to the development of human disease states remain poorly defined. Their exact function isn’t well known. C.Eosinophils their main action is to help fight infections caused by parasites. A high number of eosinophils (eosinophilia) are often linked to a variety of disorders. A high eosinophil count may be due to: Adrenal gland deficiency. Also it could mean allergic disease, including hay fever.
- II Monocytes break down and remove foreign organisms and dying cells from your body. Main action against bacterial infection. They have subsets no Types (too much for this topic). Clevaland Clinic states “Monocytes are a type of white blood cell (leukocytes) that reside in your blood and tissues to find and destroy germs (viruses, bacteria, fungi and protozoa) and eliminate infected cells. Monocytes call on other white blood cells to help treat injury and prevent infection.
- III Lymphocytes make up your immune system. Lymphocytes are a type of white blood cell. They help your body’s immune system fight cancer and foreign viruses and bacteria. Your lymphocyte count can be taken during a normal blood test at your healthcare provider’s office. Lymphocyte levels vary depending on your age, race, sex, altitude and lifestyle.
Memorial Sloan Kettering Center in NYC states “White blood cells have a wide range of lifespans, from hours to years.”.
3-Platelets (thrombocytes)
Platelets are small parts of cells. Their main function is to control bleeding. They make up a very small part of your blood (less than 1%). The lifespan of platelets is about 9 to 12 days.
4-Plasma
Plasma is the pale-yellow liquid part of your blood that holds all of your blood cells. It makes up a little over half of your total blood. On average about 5-6 liters of blood, and females average 4–5 liters.
Plasma helps move water, nutrients, minerals, medications, and hormones throughout your body. It also carries waste products to your kidneys. Then your kidneys filter out the waste products from your blood. Plasma is made up of water, protein, lipids (fats). It carries water, fat-soluble nutrients, and other substances to and from the different organs.
Plasma is 92% water. Dissolved or suspended within this water is a mixture of substances, most of which are proteins. There are hundreds of substances dissolved in the plasma, although many of them are found only in very small quantities.
Approximately 7 percent make up of plasma is protein.
The three major groups of plasma proteins are as follows:
- Albumin is the most abundant of the plasma proteins. Manufactured by the liver, albumin molecules serve as binding proteins—transport vehicles for fatty acids and steroid hormones. Recall that lipids are hydrophobic; however, binding to albumin enables their transport in the watery plasma. Albumin is also the most significant contributor to the osmotic pressure of blood; that is, its presence holds water inside the blood vessels and draws water from the tissues, across blood vessel walls, and into the bloodstream. This in turn helps to maintain both blood volume and blood pressure. Albumin normally accounts for approximately 54 percent of the total plasma protein content, or 3.5–5.0 g/dL of blood.
- The second most common plasma proteins are the globulins. A heterogeneous group, there are three main subgroups known as alpha, beta, and gamma globulins. The alpha and beta globulins transport iron, lipids, and the fat-soluble vitamins A, D, E, and K to the cells; like albumin, they also contribute to osmotic pressure. The gamma globulins are proteins involved in immunity and are better known as an antibodies or immunoglobulins. Unlike alpha and beta globulins, which are produced in the liver, immunoglobulins are produced by specialized leukocytes known as plasma cells. Globulins make up approximately 38 percent of the total plasma protein volume, or 1.0–1.5 g/dL of blood.
- The least abundant plasma protein is fibrinogen. Like albumin and the alpha and beta globulins, fibrinogen is produced by the liver. It is essential for blood clotting, a process described later in this chapter. Fibrinogen accounts for about 7 percent of the total plasma protein volume, or 0.2–0.45 g/dL of blood.
Other Plasma Solutes
In addition to proteins, plasma contains a wide variety of other substances. These include various electrolytes, such as sodium, potassium, and calcium ions; dissolved gases, such as oxygen, carbon dioxide, and nitrogen; various organic nutrients, such as vitamins, lipids, glucose, and amino acids; and metabolic wastes. All of these non-protein solutes combined contribute approximately 1 percent to the total volume of plasma.
Resources
Johns Hopkins Medicine
www.hopkinsmedicine.org/health/wellness-and-prevention/facts-about-blood
This website has facts about blood, blood cells, and blood cell count.
American Red Cross
www.redcrossblood.org
The American Red Cross offers a variety of information about the different parts of blood and what blood cells do.
Stanford Children’s Health
www.stanfordchildrens.org
Stanford Children’s Health offers a variety of information about the different parts of blood and what blood cells do.