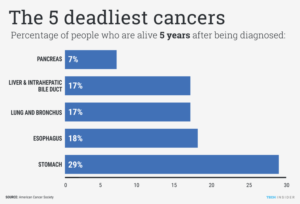
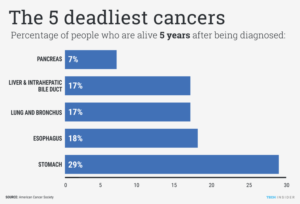
Pancreatic cancer is one of the few types of cancer that haven’t improved in terms of survival rates over the years, according to the Hirshberg Foundation for Pancreatic Cancer Research. In fact, the foundation said the mortality rate is 93-percent within 5-years of diagnosis. And 71-percent will die in first year. Usually people diagnosed with this disease are told they have 6 months to 1 year survival rate. There are the few for the many that live longer but know this the major depending factor is also the stage level of cancer your in (I, II, III & IV). The higher the worse the metastasis.
These stats point to why it’s important to raise awareness about this killer cancer, and to outline some facts and figures. In honor of Pancreatic Cancer Awareness Month in November, here are six things to know, thanks to Jeff Hayward on November 1 informed the world of this information on his blog with facts…
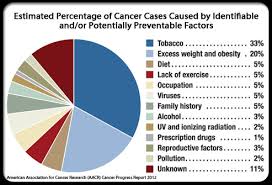
1. Their are Risk Factors
The American Cancer Society says that the average lifetime risk of developing cancer of the pancreas in both men and women is 1 in 65. However, there are certain factors that might make you more likely to face the disease.
Cancer Treatment Centers of America notes that these risk factors include age (most pancreatic cancers form at age-55 or older), gender (males are slightly more likely to develop it), obesity, diabetes, smoking, and more.
2. Heredity
Cancer Treatment Centers of America also notes that about 10-percent of pancreatic cancer cases are thought to be genetic, or passed down from a parent.
These genetic mutations include hereditary breast and ovarian cancer syndrome (BRCA2), familial melanoma (p16), familial pancreatitis (PRSS1), and neurofibromatosis type-1 (NF1), adds the source. Other “inherited syndromes” can raise risks including Lynch syndrome (hereditary nonpolyposis colorectal cancer), Peutz-Jeghers Syndrome, and Von Hippel-Lindau Syndrome.
3. There Were 50,000 Cases 2016 and NOW:
The American Cancer Society estimated in 2023 there were 53,070 new diagnoses of pancreatic cancer this year in the U.S., and sadly it adds that it expected more than 41,000 of those patients to die from it.
According to the Pancreatic Cancer Action Network report, an estimated 66,440 Americans will be diagnosed with pancreatic cancer in 2024, and 51,750 are predicted to die from the disease this year. Pancreatic cancer continues to be the third-leading cause of cancer-related death in men and women combined in the United States and is on track to become the second-leading cause before 2030.
Of those numbers, there were an estimated 27,670 men diagnosed in 2016, compared to an estimated 25,400 diagnoses for women. The death rates are proportionate for both, according to additional statistics from the cancer society.
The American Cancer Society’s estimates for pancreatic cancer in the United States for 2023 are:
- About 64,050 people (33,130 men and 30,920 women) will be diagnosed with pancreatic cancer.
- About 50,550 people (26,620 men and 23,930 women) will die of pancreatic cancer.
Pancreatic cancer accounts for about 3% of all cancers in the US and about 7% of all cancer deaths.
It is slightly more common in men than in women.
4. One of Most Prevalent Cancers in the World
The World Cancer Research Fund International notes that pancreatic cancer shares 10th-place in global prevalence with kidney cancer. Worldwide, there were 338,000 cases of pancreatic cancers diagnosed in 2012 alone, notes the source.
Looking at a breakdown of the disease’s age-standardized rates by country, the U.S. comes in 20th at 7.5-cases per 100,000. The top two countries in the world for cancer of the pancreas are Czech Republic (9.7-per 100,000) and Slovakia (9.4-per 100,000).
5. It Often Causes Symptoms When it’s Too Late
Scientific American talks about why this type of cancer is so deadly in a 2011 article making reference to Apple founder Steve Jobs, who died from the cancer.
It notes that patients sometimes don’t seek treatment right away, because symptoms including weight loss, jaundice and abdominal pain don’t begin until the later stages. “They usually start after the tumor is a significant size. By then, chances are, it has metastasized (that is, spread to other parts of the body),” explains the article.
6. There’s More than One Type
The American Cancer Society explains the overwhelmingly common form of this cancer is pancreatic adenocarcinoma, which makes up 95-percent of all cases. These begin in the ducts of the pancreas and sometimes develop from the cells that form pancreatic enzymes, according to the source.
The “other” type of cancer of the pancreas is pancreatic endocrine tumors, otherwise known as neuroendocrine tumors, explains the cancer society. These tumors can be cancerous or benign, and are subdivided into other categories including “functioning NETs” (including gastrinomas, insulinomas and glucagonomas), and “non-functioning NETs” which are actually more likely to cause cancer because they can grow larger before they’re discovered.
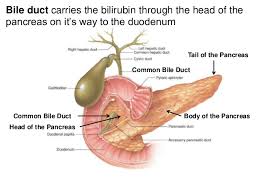
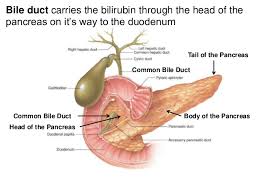
Know how it works you have a pancreas medically noted in Anatomy and Physiology as having a head, neck, body and tail. The location of the cancer can play a major role especially if diagnosed earlier, depending on the location for some.
The head is the widest part of the pancreas. The head of the pancreas is found in the right side of abdomen, nestled in the curve of the duodenum body and tail. Worse place for pancreas since this allows metastasis faster than other areas of the pancreas. The head of the pancreas is connected to other body organs and near lymph nodes making it the ideal place for metastasis (spreading) to occur. Know this in some cases caught early can make a major change in a longer life for some.
The neck is the thin section of the gland between the head and the body of the pancreas.
The body is the middle part of the pancreas between the neck and the tail. The superior mesenteric artery and vein run behind this part of the pancreas. This is not connected like the head and if caught early results can be better.
The tail is the thin tip of the pancreas in the left side of the abdomen, in close proximity with the spleen. This is the end of the pancreas connected to nothing, no ducts or other tissues or other body glands of the body that put it near by lymph nodes or connected to and best place for area of the cancer especially if it is only in the tail, in most cases, since less chance of spreading the cancer. Also if only in the tail of pancreas, surgery will entail removal of that part of the organ with chemo a few months and resolved in most cases. Just follow up visits to your chemo doctor for however long the M.D. directs you.