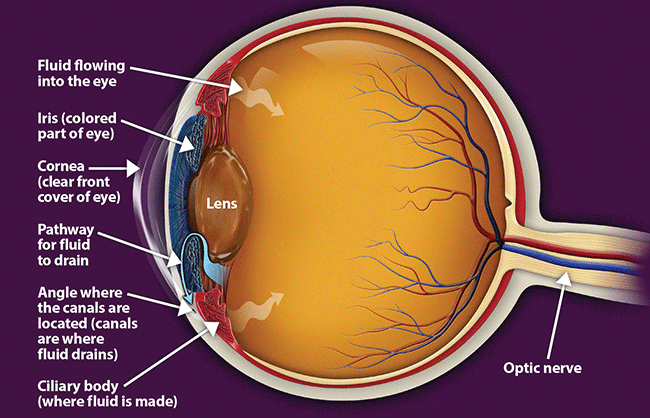
If you are diagnosed with glaucoma, it is important to set a regular schedule of examinations with your eye doctor to monitor your condition and make sure that your prescribed treatment is effectively maintaining a safe eye pressure.
Treatments
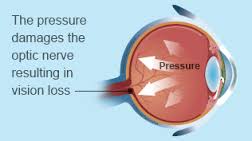
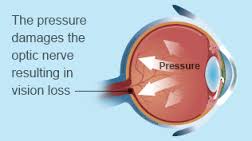
The Treatment of Glaucoma: The damage caused by glaucoma can’t be reversed. But treatment and regular checkups can help slow or prevent vision loss, especially in you catch the disease in its early stage. The goal of glaucoma treatment is to lower pressure in your eye (intraocular pressure). Depending on your situation, your options may include eyedrops, laser treatment or surgery.
Remember The damage caused by glaucoma can’t be reversed. But treatment and regular checkups can help slow or prevent vision loss, especially in you catch the disease in its early stage. The goal of glaucoma treatment is to lower pressure in your eye (intraocular pressure). Depending on your situation, your options may include eyedrops, laser treatment or surgery.
Eyedrops
Glaucoma treatment often starts with prescription eyedrops. These can help decrease eye pressure by improving how fluid drains from your eye or by decreasing the amount of fluid your eye makes. Depending on how low your eye pressure needs to be, more than one of the eyedrops below may need to be prescribed.
Prescription eyedrop medications include:
- Prostaglandins. These increase the outflow of the fluid in your eye (aqueous humor), thereby reducing your eye pressure. Medicines in this category include latanoprost (Xalatan), travoprost (Travatan Z), tafluprost (Zioptan), bimatoprost (Lumigan) and latanoprostene bunod (Vyzulta). Possible side effects include mild reddening and stinging of the eyes, darkening of the iris, darkening of the pigment of the eyelashes or eyelid skin, and blurred vision. This class of drug is prescribed for once-a-day use.
- Beta blockers. These reduce the production of fluid in your eye, thereby lowering the pressure in your eye (intraocular pressure). Examples include timolol (Betimol, Istalol, Timoptic) and betaxolol (Betoptic). Possible side effects include difficulty breathing, slowed heart rate, lower blood pressure, impotence and fatigue. This class of drug can be prescribed for once- or twice-daily use depending on your condition.
- Alpha-adrenergic agonists. These reduce the production of aqueous humor and increase outflow of the fluid in your eye. Examples include apraclonidine (Iopidine) and brimonidine (Alphagan P, Qoliana). Possible side effects include an irregular heart rate, high blood pressure, fatigue, red, itchy or swollen eyes, and dry mouth. This class of drug is usually prescribed for twice-daily use but sometimes can be prescribed for use three times a day.
- Carbonic anhydrase inhibitors. These medicines reduce the production of fluid in your eye. Examples include dorzolamide (Trusopt) and brinzolamide (Azopt). Possible side effects include a metallic taste, frequent urination, and tingling in the fingers and toes. This class of drug is usually prescribed for twice-daily use but sometimes can be prescribed for use three times a day.
- Rho kinase inhibitor. This medicine lowers eye pressure by suppressing the rho kinase enzymes responsible for fluid increase. It is available as netarsudil (Rhopressa) and is prescribed for once-a-day use. Possible side effects include eye redness, eye discomfort and deposits forming on the cornea.
- Miotic or cholinergic agents. These increase the outflow of fluid from your eye. An example is pilocarpine (Isopto Carpine). Side effects include headache, eye ache, smaller pupils, possible blurred or dim vision, and nearsightedness. This class of medicine is usually prescribed to be used up to four times a day. Because of potential side effects and the need for frequent daily use, these medications are not prescribed very often anymore.
Because some of the eyedrop medicine is absorbed into your bloodstream, you may experience some side effects unrelated to your eyes. To minimize this absorption, close your eyes for one to two minutes after putting the drops in. You may also press lightly at the corner of your eyes near your nose to close the tear duct for one or two minutes. Wipe off any unused drops from your eyelid.
If you have been prescribed multiple eyedrops or you need to use artificial tears, space them out so that you are waiting at least five minutes in between types of drops.
Oral medications
If eyedrops alone don’t bring your eye pressure down to the desired level, your doctor may also prescribe an oral medication, usually a carbonic anhydrase inhibitor. Possible side effects include frequent urination, tingling in the fingers and toes, depression, stomach upset, and kidney stones.
Surgery and other therapies
Other treatment options include laser therapy and various surgical procedures. The following techniques are intended to improve the drainage of fluid within the eye, thereby lowering pressure:
- Laser therapy. Laser trabeculoplasty (truh-BEK-u-low-plas-tee) is an option if you have open-angle glaucoma. It’s done in your doctor’s office. Your doctor uses a small laser beam to open clogged channels in the trabecular meshwork. It may take a few weeks before the full effect of this procedure becomes apparent.
- Filtering surgery. With a surgical procedure called a trabeculectomy (truh-bek-u-LEK-tuh-me), your surgeon creates an opening in the white of the eye (sclera) and removes part of the trabecular meshwork.
- Drainage tubes. In this procedure, your eye surgeon inserts a small tube shunt in your eye to drain away excess fluid to lower your eye pressure.
- Minimally invasive glaucoma surgery (MIGS). Your doctor may suggest a MIGS procedure to lower your eye pressure. These procedures generally require less immediate postoperative care and have less risk than trabeculectomy or installing a drainage device. They are often combined with cataract surgery. There are a number of MIGS techniques available, and your doctor will discuss which procedure may be right for you.
After your procedure, you’ll need to see your doctor for follow-up exams. And you may eventually need to undergo additional procedures if your eye pressure begins to rise again or other changes occur in your eye.