Ticks bite into the skin, then dig into it. Lastly, fills up the blood sac for food.

The mark the tick leaves behind on the arm it bit.

A tick typically feeds for several days until it becomes fully engorged with blood. As it fills, its body swells, changing from a flat, seed-like appearance to a plump, globular form. Once engorged, the tick naturally detaches from its host.
This detachment is usually passive; the tick simply releases its grip and falls off. After detaching, the tick seeks a secluded and protected environment. It retreats to areas like leaf litter, cracks, or crevices, where it is less vulnerable to predators or environmental extremes.
Next Stages in the Tick’s Life Cycle
The blood meal a tick consumes is fundamental for its development and reproduction. Different tick life stages have distinct outcomes following engorgement.
For larval and nymphal ticks, a blood meal is a prerequisite for molting into the next developmental stage. After feeding, a six-legged larva transforms into an eight-legged nymph, and a nymph molts into an adult. This transformation allows the tick to grow and progress, preparing it for its next blood meal.
For adult female ticks, the blood meal provides the energy and nutrients necessary for egg production. Once fully fed, a female tick detaches and seeks a sheltered location to lay her eggs. She can lay thousands of eggs, often ranging from 1,000 to 8,000, after which she typically dies.
Male ticks may take smaller, more frequent blood meals. Their primary purpose after feeding is to find a mate. The male tick feeds before mating as well, but he’s often a fraction of the size of the engorged female when mating takes place. Often, the male dies after mating, and the female dies after laying anywhere from 2,000 to 18,000 eggs. Soft ticks are an exception. Many species of soft tick eat several smaller blood meals and lay eggs several times. This is one reason soft ticks don’t consume as much blood in one sitting or swell to the extent that hard ticks do.
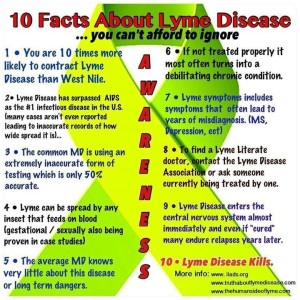
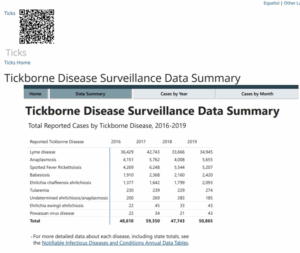
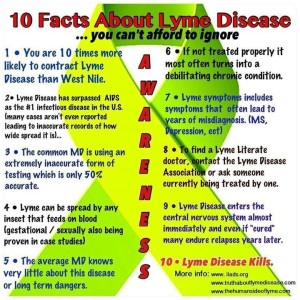
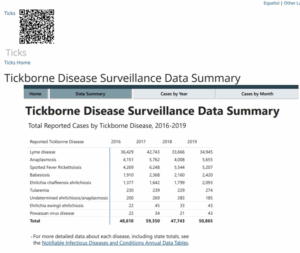
In 2013, there were more than 25,000 confirmed cases of Lyme disease reported across the country, according to the Center For Disease Control And Prevention.
Lyme disease is of course a potentially debilitating infection spread by ticks. A special conference this weekend, now in it’s fourth year — is hoping to help raise awareness.
On Saturday, September 12, the Mt. Valley Lyme Disease Awareness Coalition will hold it’s 4th Annual Lyme Conference. This year’s day long event will be held at Telstar Regional High School in Bethel and is open to the public. Donations at that door to help in their researching.
We’re constantly hearing about the threat of Lyme disease when it comes to our pets. However, sometimes it takes star power in order to bring a dangerous condition into the “Lyme-light” for humans. This is exactly what Yolanda Foster, from the reality television show, Real Housewives of Beverly Hills, and wife of composer David Foster, did after suffering unexplainable symptoms—such as emotional outbursts, nervous system abnormalities, skin issues, and loss brain function. Her diagnoses: chronic Lyme disease.
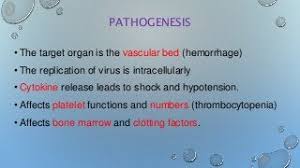
Lyme disease is a bacterial illness that is spread by the borrelia burgdorferi bacteria in tick insect bites. Once infected, the victim (human or animal) will suffer the consequences in multiple stages that stretch from the first bite to the spread of Lyme antibodies within the blood, and the symptoms.
The most common tick-borne illness in North America and Europe, Lyme disease is transmitted by the bite of an infected blacklegged tick.
The most common signs or symptoms indicating Lyme Disease:
You have flu-like symptoms
One of the common symptoms of Lyme disease is feeling like you have a flu. This means that you’ll begin suffering from a runny nose, fevers, chills, and shaking. All the symptoms you associate with the flu can also indicate that you are in the early stages of Lyme disease and it’s at this point that you should go and see a doctor.
Many people will simply brush off the conditions and take medication bought over the counter, but if you can catch the disease at this stage, it’s far simpler to treat.
You have a stiff neck
If your neck is sore and you have the above-mentioned flu-like symptoms, it’s possible that you have developed Lyme disease. A stiff neck is a really common indicator of having recently contracted the disease. The reason it begins is because of the infection traveling around the body and if you find yourself with this pain, it’s important to get checked right away. Not only that but the pain involved with it can also get worse, making it almost unbearable. At this stage you should definitely see a doctor.
Headaches
On top of the above two symptoms, headaches will usually begin when you are in the early stages of developing the condition. A checkup is essential at this stage, your doctor will be able to provide you with treatment that is more effective the sooner after you contract the disease.
Muscle numbness
Muscle numbness occurs even during the early stages of Lyme disease making it difficult to move and creating either a numbness or a tingling feeling in muscles all over the body. Another common complaint is that the individual has shooting pains that go from the top of the leg to the bottom.
These symptoms are worrisome whether you have Lyme disease or not, so be sure to speak to your doctor as soon as you start experiencing these kinds of serious symptoms.
Fatigue
One of the signature symptoms of Lyme disease that most people have heard about is fatigue. This symptom occurs later on in the disease and is actually known as ‘post-Lyme syndrome’. It is far more than just feeling tired – it makes the muscles completely incapable of moving.
Along with the fatigue, the individual will suffer great pain in their muscles, bones, and joints.
Swelling
This symptom is more common during the early stages of the disease and it includes the swelling of the muscles, joints, and anywhere else in the body. The effect occurs as the body tries to protect itself from the bacteria that has invaded. Swelling is a natural response to many conditions and, as time goes by, the individual will find that the swelling can get worse and worse.
Heart problems
If you have heart problems and your family doesn’t have a history of it, this could be an indicator that you have Lyme disease and simply haven’t realized it yet. This is far less common than other symptoms, but in some cases an irregular heartbeat can actually suggest that you have Lyme disease and left it untreated for a long period of time.
If you have an irregular heartbeat, there’s no need to assume that you have Lyme disease – but you should of course go ahead with all the tests that your doctors want you to go ahead with.
Muscle numbness
Muscle numbness occurs even during the early stages of Lyme disease making it difficult to move and creating either a numbness or a tingling feeling in muscles all over the body. Another common complaint is that the individual has shooting pains that go from the top of the leg to the bottom.
These symptoms are worrisome whether you have Lyme disease or not, so be sure to speak to your doctor as soon as you start experiencing these kinds of serious symptoms.
Bull’s eye rash
The bull’s eye rash is the first sign of Lyme disease, and it occurs around the region that the tick originally embedded itself into the skin. There are lots of ways that this rash might appear, with the first being the obvious bull’s eye shape, with a blistering lesion in the middle and surrounding circles of redness. Some lesions may have a uniform red color, others may be disseminated and others may appear blue-red. The thing to look out for is a large circular rash that appears dark red.
Facial drooping
This is one of the most serious symptoms of Lyme disease and is pretty uncommon, but it’s important to know about nonetheless. This symptom includes the dropping of the face, where muscles stop working and you find it difficult to speak. Some individuals have experienced this symptom, known as facial palsy, to the extent that it resembles a stroke. This is of course something very serious and something you should go straight to hospital about should you begin experiencing it.
Facts to know about lyme disease:
-Lyme disease is caused by bacteria called Borrelia burgdorferi that is only transmitted to humans when they are bitten by an infected tick.
-To infect its host, a tick typically must be attached to the skin for at least 36 hours.
-Most cases of Lyme disease occur in late spring and early summer.
– The most common symptoms of Lyme disease include a red, circular “bulls-eye” rash often accompanied by muscle and joint aches. About 70 to 80 percent of people infected develop the rash, which shows up several days to weeks after the tick bite.
-Lyme disease is diagnosed by medical history, physical exam, and sometimes a blood test. It may take four to six weeks for the human immune system to make antibodies against Borrelia burgdorferi and therefore show up in a positive blood test. That is why patients with the Lyme rash usually have a negative blood test and diagnosis is based on the characteristic appearance of the rash. Patients with other clinical manifestations such as Lyme arthritis will usually have a blood test. Anyone who has symptoms for longer than six weeks and who has never been treated with antibiotics is unlikely to have Lyme disease if the blood test is negative.
–Most cases of Lyme disease are successfully treated with a few weeks of antibiotics. Using antibiotics for a very long time (months or years) does not offer superior results and in fact can be dangerous, because it can cause potentially fatal complications.
-Approximately 95 percent of all cases of Lyme disease occur in the Northeast and the Upper Midwest.
-Researchers didn’t identify the cause of Lyme disease and connect it with ticks until 1981. The bacterium that causes the disease is named in honor of Willy Burgdorfer, the scientist who made the connection.
-There were nearly 30,000 confirmed cases of Lyme disease in 2009 and more than 8,500 probable cases. The number has risen steadily since 1995, when there were only 11,700 confirmed cases.
– The best treatment for Lyme disease is prevention: Be cautious when walking in the woods, avoiding bushy and grassy areas. Wear long pants and long-sleeved shirts and wear insect repellent containing DEET on exposed skin. After walking in wooded areas, thoroughly check the skin for ticks! Today in 2022 CDC states “A new active ingredient, discovered and developed by the Centers for Disease Control and Prevention (CDC), has been registered by the Environmental Protection Agency (EPA) for use in insecticides and insect repellents.
The new ingredient, nootkatone, repels and kill ticks, mosquitoes, and a wide variety of other biting pests. Nootkatone is responsible for the characteristic smell and taste of grapefruit and is widely used in the fragrance industry to make perfumes and colognes. It is found in minute quantities in Alaska yellow cedar trees and grapefruit skin.
Nootkatone can now be used to develop new insect repellents and insecticides for protecting people and pets. CDC’s licensed partner, Evolva, is in advanced discussions with leading pest control companies for possible commercial partnerships. Companies interested in developing brand name consumer products will be required to submit a registration package to EPA for review, and products could be commercially available as early as 2022.
“CDC is proud to have led the research and development of nootkatone,” said Jay C. Butler, MD, Deputy Director for Infectious Diseases. “Providing new alternatives to existing bite-prevention methods paves the way to solving one of biggest challenges in preventing vector-borne diseases—preventing bites.”
The E.P.A. has approved nootkatone, which is found in cedars and grapefruit. It repels ticks, mosquitoes and other dangerous bugs for hours, but is safe enough to eat.