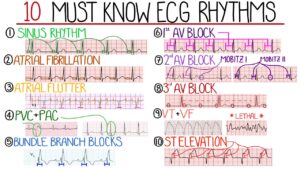
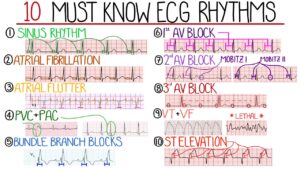
The rhythms above are heart blocks (HB) that occur in the bottom of the upper chambers which can occur in some people. There is 1st degree HB where you can live a completely normal life with but 2nd and 3rd degree HB needs treatment (usually a pacemaker) by cardiologist surgeon. After treatment with 2nd and 3rd degree HB you can live a completely normal life with follow up with your cardiologist and yearly pacemaker checks.
In this rhythm below the Ventricular Tachycardia is with a point on the top but than flips upside down (commonly called Torsedes Pointes). This is commonly due to Magnesium Level low and IV Magnesium in the hospital is given 1 to 2 gm.
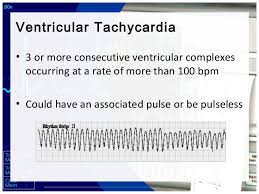
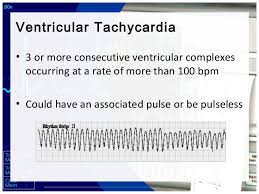
This rhythm above with a pulse=also a rhythm pulsating in different areas of the heart in the ventricles only causing the rhythm not to look identical throughout the tele strip above = Polymorphic V- Tac- meaning the stimulus in the ventricles to make the heart beat is coming from different areas of the ventricles for each beat. Each jagged tooth is a beat that makes up the whole strip shown above for Ventricular Tachycardia.
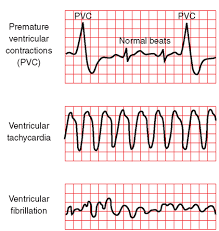
Than when the atriums aren’t working as the natural pacemaker that took over for the sinus node but now they don’t work so now the ventricles take over and the rhythms of all ventricle rhythms are with NO p waves since the atriums are not working so no p wave is involved but we have QRS waves but their wide in measurement because the rhythm starts in the ventricles. The rhythms are PVC (Premature Ventricular Contractions), Idioventricular Rhythm, Ventricular tachycardia (Monomorphic and Polymorphic-rhythm getting more irregular. When regular and monomorphic=looking identical with every ventricular beat or contraction as opposed to polymorphic=not looking identical each contraction but each one is a ventricular contraction), Torsades De Pointes Ventricular Tachycardia (the rhythm starts upright but turns upside down but each contraction without a p wave and a wide contraction meaning a ventricular contraction), and Ventricular Fibrillation, to asystole.
Here’s what they look like:
Accelerated Idioventricular Rhythm
Accelerated idioventricular rhythm occurs when three or more ventricular escape beats appear in a sequence. Heart rate will be 50-100 bpm. The QRS complex will be wide (0.12 sec. or more).
A regular QRS measures less than 0.12 which is with all atriums rhythms.
Asystole
Asystole is the state of no cardiac electrical activity and no cardiac output. Immediate action is required.
Idioventricular Rhythm
Idioventricular rhythm is a slow rhythm of under 50 bpm. It indicates that then ventricules are producing escape beats.
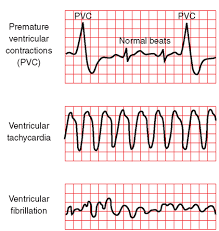
Premature Ventricular Complex-PVC (above 1st strip in #4)
Premature ventricular complexes (PVCs) occur when a ventricular site generates an impulse. This happens before the next regular sinus beat. Look for a wide QRS complex, equal or greater than 0.12 sec. The QRS complex shape can be bizarre. The P wave will be absent.
Premature Ventricular Complex – Bigeminy a QRS after every 2 regular beats
Premature Ventricular Complex – Trigeminy a QRS after every 3 regular beats
Premature Ventricular Complex – Quadrigeminy a QRS after every 4 regular beats
The more PVC’s especially right next to each other can lead to Ventricular Tachycardia to Ventricular Fibrillation if not treated in time.
Ventricular Fibrillation (in above strip-3rd one)
Ventricular fibrillation originates in the ventricules and it chaotic. No normal EKG waves are present. No heart rate can be observed. Ventricular fibrillation is an emergency condition requiring immediate action.
Ventricular Tachycardia (in above strip-2nd one)
A sequence of three PVCs in a row is ventricular tachycardia. The rate will be 120-200 bpm. Ventricular Tachycardia has two variations, monomorphic and polymorphic. These variations are discussed separately.
Ventricular Tachycardia Monomorphic
Monomorphic ventricular tachycardia occurs when the electrical impulse originates in one of the ventricules. The QRS complex is wide. Rate is above 100 bpm. Each V tac beat looks identical like in the strip above.
Ventricular Tachycardia Polymorphic
Polymorphic ventricular tachycardia has QRS complexes that very in shape and size. If a polymorphic ventricular tachycardia has a long QT Interval, it could be Torsade de Pointes. The strip shows the pulses are not identical=polymorphic since the pulse beats are coming from all different areas of the ventricles.
Torsade de Pointes (the rhythm strip at the top under Heart Blocks)
Torsade de Pointes is a special form of ventricular tachycardia. The QRS complexes vary in shape and amplitude and appear to wind around the baseline. This is an example or polymorphic ventricular tachycardia.
Ventricular ending line needs to be treated stat to be switched back to atrial rhythm since the heart is missing ½ of the conduction it’s to normally receive from the atriums and if not reversed the heart will go into failure to heart attack or to asystole flat line and go into a cardiac arrest.
With PVCs=Premature Ventricle Contractions asymptomatic we just closely monitor the pt and telemetry the pt is on. Now a pt with PVCs and symtomatic usually meds with 0xygen (sometimes 02 alone resolves it but other times with meds) but if it gets worse into V Tachycardia the treatment is below.
Idioventricular Rhythm (IVR)is usually with a slow brady pulse and needs meds. Accelerated IVR (AIVR) is usually hemodynamically tolerated and self-limited; thus, it rarely requires treatment.
Occasionally, patients may not tolerate AIVR due to (1) loss of atrial-ventricular synchrony, (2) relative rapid ventricular rate, or (3) ventricular tachycardia or ventricular fibrillation degenerated from AIVR (extremely rare). Under these situations, atropine can be used to increase the underlying sinus rate to inhibit AIVR.
Other treatments for AIVR, which include isoproterenol, verapamil, antiarrhythmic drugs such as lidocaine and amiodarone, and atrial overdriving pacing are only occasionally used today.
Patients with AIVR should be treated mainly for its underlying causes, such as digoxin toxicity, myocardial ischemia, and structure heart diseases. Beta-blockers are often used in patients with myocardial ischemia-reperfusion and cardiomyopathy
With Ventricular rhythms with fast pulse over 100 with symptomatic signs for the patient we may use as simple as valsalva pressure on the neck that medical staff only do but when pt is in asymptomatic (no symptoms) Ventricular Tachycardia (V-Tac) to even medications but when symptomatic if in V-Tac start cardioversion with a pulse if no pulse called pulseless V-Tac we use a defibrillator since there is no pulse there is no QRS to pace with in having the shock hit at the R wave, why? NO PULSE.
Treatment for Torsade de Pointes is Magnesium deficiency and Mag. Supplement given IV 2gms. Usually effective but if necessary the same as above as directed for it with a pulse or the other V Tac. (without a pulse)-See above.
Ventricular Fibrillation is when the ventricles are just quivering and the atriums in any ventricular rhythm doing nothing. The pt needs CPR and ASAP a defibrillator in hopes the shock will knock the rhythm back to a normal sinus or some form of a real rhythm.
Asystole which is a straight line, no pulse and this is CPR with epinephrine or Vasopressin 40 for only the replacement of the 1st or 2nd dose of Epinephrine 1mg. This is given 3-5 minutes (epinephrine). No defibrillation since no pulse. A rhythm may come back and if not the MD will call when CPR stops. Asystole is hard to resolve in most cases highier probability of resolution if in a hospital where close monitoring is done and its detected quicker.
The PURPOSE in treating any rhythm abnormal to the human heart is to reach the goal of a optimal or healthiest rhythm (a normal sinus rhythm , the best rhythm the heart can be in) and if not reaching an atrial rhythm. We the medical field aim to reach a heart rhythm the patient can live with and hopefully reaching the best NSR-Normal Sinus Rhythm. Normal sinus rhythm that is a rhythm starting from the upper right chamber extending to the left one and continues down on both sides to the bottom of the ventricles. This rhythm is giving the most effective oxygen perfusion to the heart to allow it to do its function (pumping good oxygenated blood flow out of the left ventricle at the same time pumping highly carbon dioxide blood from the right side of the heart to the lungs to get more oxygen). Doing this it allows the human body to get good amounts of oxygen to all our tissues=good overall oxygen perfusion to all tissues. At the same time what happens is red blood cells from all tissues with mostly used up oxygen from the cell and more carbon dioxide in the cell are also being pumped by the heart to return to the right side to the lungs to go through this whole process again in getting more oxygen in the RBCs which keeps us alive. A human without oxygen or low oxygen to their tissues or any tissue is going to reach cellular starvation which in turn causes starvation to the tissues (in general) or to a tissue area (Ex. Take the diabetic-regarding the foot to lack of 02 to cyanotic purple tissue to necrotic black tissue=dead to amputated since the tissue is dead. Remember by gravity the foot is the furthest from the heart).
Cardiac Arrest or Heart Attack are more likely to occur in a irregular rhythm especially making the heart work to hard being RVR afib in the atriums that can lead easily to ventricular tachycardia to ventricular fibrillation and not treated immediately.
Cardiac Arrest or an abnormal heart rhythm is an electrical problem with the conduction of the heart whereas a Heart Attack can be caused by a blockage of blood. An example could be the coronary arteries-main arteries of oxygenated blood to the heart that can lead to a bad rhythm due to lack of 0xygen that leads to worse rhythms as the heart gets more stressed out.
For direction many experts like Atlantic Endocrinology states the following:
“You feel fine—no chest pain, no shortness of breath, no obvious red flags. But what if heart disease is developing silently? It does for many where the cardiac condition was there awhile but no symptoms and the symptoms arise when the condition gets worse for many cardiac Dx’s. Who wants to go to the doctor when they feel fine but there is always the silent symptoms and not just for cardiac issues but for this topic we will keep to just cardiac issues.
Many people assume a cardiologist is only for the elderly or those with symptoms, yet heart issues often start long before warning signs appear. So, when is the right time to schedule that first cardiac appointment? The answer might be earlier than you think.
Seeing a cardiologist isn’t just for the elderly or those with symptoms—heart disease can develop silently. Men over 40 and women after menopause face increased risk, especially with a family cardiac history of heart disease, high blood pressure, cholesterol, or diabetes. Preventive check-ups before age 60–70 improve outcomes.
Warning signs could definitely be such as chest pain or chest discomfort, shortness of breath or difficulty breathing, continuous headaches, palpitations continuous or intermittent, fatigue, dizziness or swelling or edema, require medical attention. Monitoring blood pressure, cholesterol, and managing lifestyle factors like diet, exercise, and stress are crucial. Those with hereditary or pre-existing heart conditions should see a cardiologist early for specialized care and prevention.”
Now even with rhythms that could lead to a heart attack! Not that the rhythms were the primary cause of the heart attack but in most cases the rhythm is due to the cardiac condition.
Now the rhythm can be used in helping the doctor as a preventative measure if found earlier enough to stop the heart attack from occurring!
Now you know why there are many reasons to see a cardiologist at least yearly from 40 and up in men and post-menopausal in women! Gave some examples or I would be writing a few novels!