EYES and how our health is vital in keeping the eyes working EFFECTIVELY.
Like all organs if your diet is not healthy you’ll effect their functioning, including your eyes. Take for example the ingredients you include in the foods & fluids you eat. Just like how some drink from one up to three thousand cc’s of water a day to help prevent dehydration in their tissues if they work out daily from a gym to running miles outside OR take someone who simply includes calcium in their diet for their bones. Well what is good for the eyes and what can you do to help both your eyes?
Get an annual comprehensive dilated eye exam. Why? During a comprehensive dilated eye exam, your eye care professional places drops in your eyes to dilate, or widen, the pupil to allow more light to enter the eye the same way an open door lets more light into a dark room. This dilation enables
your eye care professional to get a good look at the back of the eyes and examine them for any signs of damage or disease. Your eye care professional is the only one who can determine if your eyes are healthy and if you are seeing your best. That is why a yearly comprehensive eye exam is vital!
You should know your families eye history since many eye diseases are through heredity, eat an eye healthy & well-balanced diet rich in salmon, tuna, dark leafy greens, colored vegetables and fruits, wear sunglasses with UV protection and avoid smoking (which effects the body everywhere, including the eyes).
So talk to your family members about their eye health history. It’s important to know if anyone has been diagnosed with a disease or condition since many are hereditary. This information will help to determine if you are at higher risk for developing an eye disease or condition.
What ingredients do we need in our dieting that is so vital for the eyes to stay at their healthiest level?
You’ve heard carrots are good for your eyes. But eating a diet rich in fruits and vegetables, particularly dark leafy greens such as spinach, kale, or collard greens, is important for keeping your eyes healthy, too. Research has also shown there are eye health benefits from eating fish high in omega-3 fatty acids, such as salmon, tuna, and halibut.
Well Lutein and Zeaxanthin (Pronounced loo’teen and Zee’-a-zan-thin)-Powerful antioxidants naturally present in the macula (the part of the retina that is responsible for central vision). Remember damage to the retina causes some degree of lack of vision to 100% blind. Lutein and Zeaxanthin are critical for helping to filter out harmful blue light, which can damage the macula. These vital antioxidants cannot be produced by our bodies on their own, so they must be obtained through diet and/or supplements (ex. Ocuvite Supplements in the store).
Another ingredient we need in our diet is Omega 3 Fatty Acids which is a family of fatty acids that help protect our eyes by keeping them healthy. Omega 3 is an important structural lipid in the retina and helps support proper function; and is vital for the health of your eyes as you age. Lastly it helps promote healthy tear production necessary for healthy and comfortable eyes.
Other Nutrients Antioxidants Vitamins C and E, Zinc and beta carotene. They help protect eyes from oxidative stress (Oxidative stress reflects an imbalance between the systemic manifestation of reactive oxygen species and a biological system’s ability to readily detoxify the reactive intermediates or to repair the resulting damage and oxidative stress can cause disruptions in normal mechanisms of cellular signaling. It is thought to be involved in the development of many diseases.)
What Your Diet or Daily Health Habits May Be Missing:
–Many dark leafy greens and brightly colored vegetables (including orange foods) are rich in Lutein and Zeaxanthin. We all heard about carrots (to get Beta-carotene)
–Oil-rich fish such as tuna and salmon along with nuts and fortified eggs are an excellent source of omega-3s. Omega-3s: A family of fatty acids that help protect the eye to keep it healthy, another important nutrient for your eyes
Unfortunately, many of us do not consume enough of these eye-healthy foods in our daily diets. What should you have in your diet to eat per day to equal the amount of Lutein and Zeaxanthin you should have daily: 5 cups of broccoli, 6 cups of corn, 1 ounce of salmon or 4 ounces of tuna. A lot of vegetables in cups but if you mix your foods in the 4 food groups that are healthy for the eye or just simply take supplements that your doctor recommends for eye health you won’t be eating cups and cups of vegetables if you don’t like the taste.
*Know other foods high in omega 3 are halibut, spinach, collard and kale.
VITAL NUTRIENTS FOR GETTING THE EYES HEALTHY.
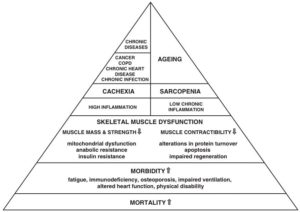
Many eye diseases can’t be avoided (like born blind) but there are many diseases that could have been avoided through prevention tactics in what you eat and in what you practice as your daily habits. For example some that could be prevented if not slowed down or suppressed in the intensity of the disease can be Age-Related Macular Degeneration, Cataracts, Dry Eye Syndrome and more.
Factors that also influence how our eyes turn out are:
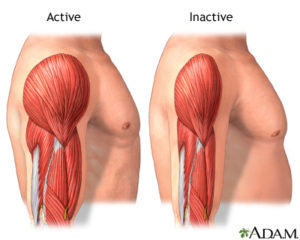
–Being overweight or obese is a factor that increases your risk of developing diabetes and other systemic conditions which can lead to vision loss, such as diabetic eye disease (macular degeneration) or even glaucoma. If you’re having trouble maintaining a healthy weight, talk to your doctor or go to my website with Dr. Anderson available to help you understand how the body works with calories/sugars, carbohydrates, starches, fats, and sugars; with understanding how portions of meals work with digestion and how it can put weight on the body.
–If you do a lot of work daily on a computer or on any one thing, your eyes may forget to blink or get very fatigued, so attempt to do every 20 minutes looking away from the computer or one thing your focused on for hours (like at work) for 20 seconds. This helps your eyes in reducing eyestrain (it is an actually an exercise for the eye).
–Clean your hands and your contact lenses properly. This is to avoid local infection in the eye. Always wash your hands before putting in and taking out the contact lenses. Follow your doctors and contact lenses website in keeping your eyes healthy and safe with using their service for your lenses.
–Practice workplace eye safety as their organization policy and procedure states but also use common sense with wearing eye goggles when doing work around the house that puts you at risk for eye damage (like weed whacking, painting, using saws etc…) Wear protective eyewear when playing sports or doing activities around the home. Protective eyewear includes safety glasses and goggles, safety shields, and eye guards specially designed to provide the correct protection for a certain activity. Most protective eyewear lenses are made of polycarbonate, which is 10 times stronger than other plastics. Many eye care providers sell protective eyewear, as do some sporting goods stores.
Also know at home to be protective and wear protective eyewear when playing sports or doing activities around the home. Protective eyewear includes safety glasses and goggles, safety shields, and eye guards specially designed to provide the correct protection for a certain activity. Most protective eyewear lenses are made of polycarbonate, which is 10 times stronger than other plastics. Many eye care providers sell protective eyewear, as do some sporting goods stores.
Our health care system is in a disaster but gradually improving and lets add to improving it for us now and ten years from now and for future generations to decrease the amount of disease and illness in our country with giving our government a reason to decrease the price in our health care system (including insurances). Please if you have any diseases or illnesses on your mind with questions that you have let me know in my comment section and I will personally try to make it the next article if not sometime that week. Thank you for reading my post.
References: 1.)http://www.ocuvite.com
Updated on 7/27/25