Treatments for Epilepsy:
1.) Medications:
Anti-seizure medication works best if taken regularly, around the same time each day. The aim of treatment is to stop all of your seizures with the lowest dose of the fewest number of ASMs and with the least side effects. Usually treatment starts using a single ASM at a low dose, which is increased slowly (called titration), until your seizures are controlled. Titration meaning the MD first starts you on a therapeutic dose for you age and body weight. If the dosage is not working he or she will increase till control of the seizure is accomplished. If your seizures are not controlled with this drug, a different ASM is usually tried (by adding in the new drug and then slowly withdrawing the first one, again doing titration-you can never stop ASMs abruptly since you would be at a high risk of a seizure). If your seizures are not controlled with a single drug, another drug might be added, so that you take two different ASMs each daye, which is not uncommon.
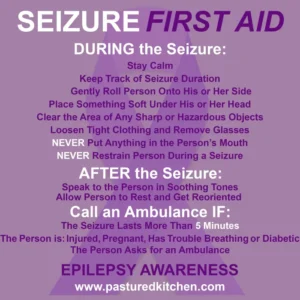
Most people’s seizures last the same length of time each time they happen and usually stop by themselves. However, sometimes seizures do not stop or one seizure follows another without the person recovering in between. When a seizure goes on for 5 minutes or more it is called status epilepticus (or ‘status’ for short).
Status during a tonic clonic (convulsive) seizure is a medical emergency and needs urgent treatment. Emergency medication is usually prescribed(like Valium through a IV site to do a intravenous push) to stop seizures once they have started and if they are going on longer than usual, or if someone has one seizure after another without recovering in between they maybe on a IV drip with IVPs till controlled. Specialist training is needed to give emergency medication.
Than there are also Medication trials:
At any time, a patient may be invited to participate in a trial of an experimental medication. Since about 1993, this is how all medications have received FDA approval. Often, patients are invited to join a trial after they have failed a number of other FDA-approved medications.
The advantages of participating in a clinical trial include:
● Access to new medication
● Close support and follow-up with the epilepsy team
● The opportunity to help medical researchers develop new treatments
The goal of medication clinical trials is to make sure the drugs are safe and effective. Clinical trials are experimental studies, so there is some risk involved with participating. However, clinical research teams follow extremely strict federal, state, and hospital guidelines to ensure that the risks are minimized.
Since there are so many anti-epilepsy drugs (AEDs) out there, it can get confusing talking to your doctor and pharmacist about them. Here is a list of seizure medications listed to help you understand the seven most widely used Anti-epileptic Drugs-AEDs in the US that are FDA approved.
7 most common seizure medications used for epilepsy:
When you are first diagnosed with epilepsy, your doctor will usually try to treat the condition with medication. The seven AEDs in this list are the most common ‘first line’ medications used for different kinds of epilepsy.
For some people, these ‘first line’ drugs work right away. But for others, the AED either doesn’t work, or the seizure medication side effects are very unpleasant. If so, their doctor will normally try an alternative medicine. For about one-third of people with epilepsy, medication doesn’t work. Fortunately, there are other treatment options available.
1. Valproic Acid
Brand names: Depakote, Depakene
Form: Can be taken as tablets, liquids, or granules (sprinkled on food)
Treats: Generalized, focal, absence – effective with most kinds of epilepsy
Since being introduced in 1978, Valproic Acid has become the most widely prescribed AED in the world. You will usually take it once or twice per day, in varying doses, depending on your age and weight.
Valproic Acid works by making it hard for your brain cells to work as fast, which means they can’t ‘fire’ off as much during a seizure.
2. Lamotrigine
Brand names: Lamictal
Form: Comes as tablets you can swallow or chew
Treats: Generalized (tonic clonic) seizures; atonic seizures
Lamotrigine is a widely used seizure medication among people with generalized epilepsy. You’ll take the tablets once or twice per day. It works by slowing down the bursts of electrical signals in the brain that happen during a seizure. Lamotrigine appears to be one of the safer AEDs to take during pregnancy – unlike many other AED medications.
3. Topiramate
Brand names: Topamax
Form: Comes as tablets to swallow
Treats: Generalized (tonic clonic) seizures; atonic seizures; Lennox-Gastaut syndrome
Topiramate is mainly used to treat generalized epilepsy. You’ll usually take the tablets twice per day. Like with other AEDs, it works by slowing down how fast your brain cells work, which helps stop seizures from developing. It should not be used if you are pregnant.
4. Carbamazepine
Brand names: Tegretol, Curatil
Form: Comes as tablets, liquids and suppositories
Treats: Focal seizures
Carbamazepine is a sodium channel blocker which was first approved to treat epilepsy in 1968. Sodium ion channels work a bit like gates in the brain, so by blocking them carbamazepine slows down how quickly signals get sent. It should not be used if you are pregnant.
5. Phenytoin
Brand names: Dilantin
Form: Comes as tablets for swallowing or chewing tablet and as a liquid
Treats: Focal seizures
Phenytoin was first approved by the FDA in 1939. It is believed to work by blocking sodium ion channels in the brain, and therefore stops high frequency firing of electric signals in the brain.
6. Oxcarbazepine
Brand names: Trileptal, Oxtellar XR
Form: Comes as tablets form, or as a liquid
Treats: Focal seizures
Oxcarbazepine is used to treat focal seizures and comes in quick and slow release forms. It’s not fully known how this AED works, but it’s believed that it blocks sodium channels in the brain.
7. Ethosuximide
Brand names: Zarontin
Form: Comes as tablets for or as a liquid
Treats: Absence seizures
Ethosuximide is a seizure medicine which is mainly used for the treatment of absence seizures, especially for children. We still don’t know quite how it works, but it seems to stop brain cells from firing so fast.
Over the past hundred years, scientists have discovered many powerful and effective AEDs which help many people lead seizure-free lives. These advances are great news for the epilepsy community as a whole. But many people who take AEDs find that they just don’t work for them – about one third of people have “refractory epilepsy”, which means they’ve tried two or more AEDs without being able to control their seizures. So about 30 percent or slight more of epilepsy patients unfortunately do not respond to their AED meds.
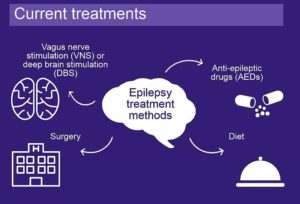
The good news is that there are several alternative ways of treating epilepsy if AEDs don’t seem to work. These include special diets and medical devices. Ending line alternate treatment levels of controlling Epilepsy! That is this weekend’s topic, Hurray!