Archive | November 2023
QUOTE FOR WEDNESDAY:
“Based on fair evidence, excessive salt intake and deficient dietary consumption of fresh fruits and vegetables are associated with an increased risk of gastric cancer. Dietary intake of vitamin C contained in vegetables, fruits, and other foods of plant origin is associated with a reduced risk of gastric cancer. Diets high in whole-grain cereals, carotenoids, allium compounds, and green tea are also associated with a reduced risk of this cancer. However, it is uncertain if changing one’s diet to include more vegetables, fruits, and whole grains would reduce the risk of gastric cancer.”
National Cancer Society (https://www.cancer.gov/types/stomach/hp/stomach-prevention-pdq)
Part III National Stomach Cancer Awareness Month – How to prevent it and treatments!
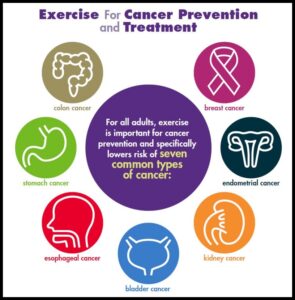
Measures for Prevention of Stomach (Gastric) Cancer Risk:
Smoking cessation
Based on solid evidence, smoking is associated with an increased risk of stomach cancer. The 2004 Surgeon General’s report identifies cigarette smoking as a cause of stomach cancer, with an average relative risk (RR) in former smokers of 1.2 and in current smokers of 1.6. Compared with persistent smokers, the risk of stomach cancer decreases among former smokers with time since cessation. This pattern of observations makes it reasonable to infer that cigarette smoking prevention or cessation would result in a decreased risk of gastric cancer.
H. pylori infection eradication
Based on solid evidence, H. pylori infection is associated with an increased risk of gastric cancer.
Treat stomach infections. If you have ulcers from an H. pylori infection, get treatment. Antibiotics can kill the bacteria, and other drugs will heal the sores in the lining of your stomach to cut your risk of cancer.
Diet
Eat healthy. Get more fresh fruits and vegetables on your plate every day. They’re high in fiber and in some vitamins that can lower your cancer risk. Avoid very salty, pickled, cured, or smoked foods like hot dogs, processed lunch meats, or smoked cheeses. Keep your weight at a healthy level, too. Being overweight or obese can also raise your risk of the disease.
Based on fair evidence, excessive salt intake and deficient dietary consumption of fresh fruits and vegetables are associated with an increased risk of gastric cancer. Dietary intake of vitamin C contained in vegetables, fruits, and other foods of plant origin is associated with a reduced risk of gastric cancer. Diets high in whole-grain cereals, carotenoids, allium compounds, and green tea are also associated with a reduced risk of this cancer. However, it is uncertain if changing one’s diet to include more vegetables, fruits, and whole grains would reduce the risk of gastric cancer.
TREATMENTS FOR STOMACH CANCER:
Many treatments can fight stomach cancer. The one you and your doctor choose will depend on how long you’ve had the disease or how much it has spread in your body, called the stage of your cancer.
Surgery. Your doctor might remove part of your stomach or other tissues nearby that have cancer cells. Surgery gets rid of the tumor and stops cancer from spreading to other parts of your body. If your disease is in a more advanced stage, your doctor might need to remove all of your stomach=Gastrectomy or in some other cases the Surgeon may only have to remove part of the stomach=Partial Gastrectomy.
Some tumors can keep food from moving in and out of your stomach. In that case, you might have surgery to put in a stent, a device that keeps the pathways open.
Chemotherapy. Drugs kill your cancer cells or keep them from growing. You can take them as pills or through an IV at a clinic. Chemo usually takes several weeks. The drugs can cause side effects, but your doctor can help you find ways to feel better during treatment.
Radiation. High-energy waves or particles can kill cancer cells and shrink tumors. Your doctor may use an X-ray or other machine to beam radiation at the spot where your tumor is.
Chemoradiation. Your doctor might use this mix of chemotherapy and radiation to shrink your tumor before surgery.
Targeted drugs. These newer drugs are different because they fight only cancer cells. Other treatments, like chemo and radiation, can kill healthy cells along with diseased ones. As a result, targeted therapies have fewer side effects than these other treatments.
QUOTE FOR TUESDAY:
“Stomach cancer is the fifth most common cancer worldwide. It is more common in countries in East Asia, Eastern Europe, and South and Central America than in the United States and other Western countries. There are many known risk factors for stomach cancer (also called gastric cancer), but often it’s not clear exactly how these factors might affect how cells in the stomach become cancer cells. This is the subject of ongoing research.”
American Cancer Society (https://www.cancer.org/cancer/types/stomach-cancer/causes-risks-prevention/what-causes.html)
Part II National Stomach Cancer Awareness Month – Risk Factors!
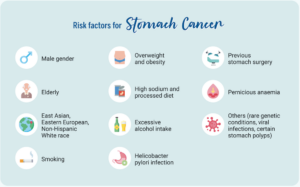
RISK FACTORS FOR STOMACH CANCER:
GENERAL
- Age: Stomach cancer is found most often in people over age 55.
- Gender: The disease affects men twice as often as women.
- Race: Stomach cancer is more common in African Americans than in Caucasians.
- Region: This type of cancer is more common in some parts of the world, such as Japan, Korea, parts of Eastern Europe and Latin America. People in these areas eat many foods that are preserved by drying, smoking, salting or pickling.
BODY
- Obesity: Obesity has been linked to an increased risk of stomach cancer
GENETICS
Certain gene mutations and some inherited conditions are considered stomach cancer risk factors. They include:
- BRCA1 & BRCA2: Inherited mutations on the BRCA1 and BRCA2 genes are often associated with higher risks for breast cancer. Individuals who have inherited these genetic mutations are also at an increased risk for stomach cancer
- E-cadherin/CDH1: Though rare, people who inherit this genetic mutation have a 70 to 80 percent chance of developing stomach cancer in their lifetime. Also, women with this genetic defect have an increased risk of breast cancer.
- Lynch syndrome: This condition may also be referred to as hereditary non-polyposis colorectal cancer (HNPCC), a genetic condition that runs in families. More commonly, this condition is associated with an increased risk for colon cancer. HNPCC also predisposes people to stomach cancers.
- Familial adenomatous polyposis (FAP): This syndrome causes polyps in the colon, stomach and intestines. Often caused by mutations of the gene APC, this syndrome greatly increases a person’s risk of colorectal cancer and may play a small role in increasing a person’s stomach cancer risk.
LIFESTYLE
- Smoking: There is evidence linking cigarette smoking to many types of cancer, including stomach cancer. Smokers have been found to be at greater risk of developing cancer than non-smokers.
- Diet: Scientists believe that eating foods preserved in these ways may play a role in the development of stomach cancer. On the other hand, fresh foods (especially fresh fruits and vegetables and properly frozen or refrigerated fresh foods) may protect against this disease.
- Working in the coal, metal or rubber industries: Chemicals that are released in these environments have been linked to the development of stomach cancer.
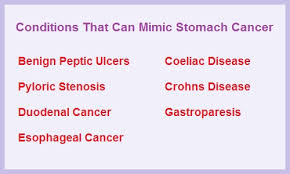
OTHER CONDITIONS
- H. pylori infection: Doctors have found that a long-term H. pylori infection may lead to inflammation and pre-cancerous changes to the stomach lining. In fact, stomach cancer patients typically have a higher incidence of H. pylori infections than people who do not have stomach cancer.
- Pernicious anemia: Some people with pernicious anemia may have gastric polyps, which can increase the risk of stomach cancer.
- Epstein-Barr virus infection: According to the American Cancer Society, Epstein-Barr virus is found in the cancer cells of about 5% to 10% of people with stomach cancer.
ENVIRONMENTAL AND OCCUPATIONAL EXPOSURES
The risk of stomach cancer is increased in people who
-
work in the rubber or coal industry
-
have been exposed to very high levels of radiation
Those at risk for Stomach Cancer:
People at elevated risk for gastric cancer include older adults with atrophic gastritis or pernicious anemia; patients with sporadic gastric adenomas, familial adenomatous polyposis, or hereditary nonpolyposis colon cancer; and immigrant ethnic populations from countries with high rates of gastric carcinoma. Workers in the rubber and coal industries are also at increased risk.
There is consistent evidence that Helicobacter pylori infection, also known as H. pylori infection, of the stomach is strongly associated with both the initiation and promotion of carcinoma of the gastric body and antrum and of gastric lymphoma.
There is consistent and solid evidence that Epstein-Barr virus (EBV) infection is strongly associated with gastric cancer.
Compared with the general population, people with duodenal ulcer disease may have a lower risk of gastric cancer.
Risk factors for gastric cancer include the presence of precursor conditions such as chronic atrophic gastritis and intestinal metaplasia, pernicious anemia, and gastric adenomatous polyps. Risk factors could include type A blood type. Environmental factors include low consumption of fruits and vegetables; consumption of salted, smoked, or poorly preserved foods; cigarette smoking; and radiation exposure.
Those at great increased risk for stomach cancer:
Hereditary diffuse gastric cancer (HDGC) is a rare inherited condition in which people have a greatly increased risk of stomach cancer, which often develops at a fairly early age. This rare syndrome is most often caused by an inherited mutation in the CDH1 gene.
It’s very important to recognize people and families with this inherited syndrome, because most people who have it will develop stomach cancer. Families with HDGC typically have two or more close relatives who develop stomach cancer (usually the diffuse type), and/or at least one person who is diagnosed before age 50. Some family members might also develop invasive lobular breast cancer.
Doctors often refer people who might have HDGC to a genetics professional, so they can discuss possibly getting genetic testing. If testing is done and shows a person has a mutation (abnormal change) in the CDH1 gene, doctors often recommend they consider having their stomach removed (typically between the ages of 20 and 30) before cancer develops. However, this operation (called a total gastrectomy) can lead to long-term changes in the way a person eats.
Some other hereditary cancer syndromes are also linked with an increased risk for stomach cancer, including Lynch syndrome, familial adenomatous polyposis (FAP), Li-Fraumeni syndrome, and Peutz-Jeghers syndrome. The risk of stomach cancer with these syndromes is not nearly as high as it is with HDGC, so removal of the stomach is not typically recommended for people who have these syndromes.
QUOTE FOR MONDAY:
“Stomach cancer can happen in any part of the stomach. In most of the world, stomach cancers happen in the main part of the stomach. This part is called the stomach body.
In the United States, stomach cancer is more likely to start by the gastroesophageal junction. This is the part where the long tube that carries food you swallow meets the stomach. The tube that carries food to the stomach is called the esophagus.
There is adenocarcinoma stomach cancer, gastrointestinal stromal tumors (GIST), carcinoid tumors – that are found in many area of the body that start in your neuroendocrine cells, and lymphoma is a cancer that starts in immune system cells. Most lymphomas that start in the stomach are a type of non-Hodgkin’s lymphoma.”
MAYO CLINIC (https://www.mayoclinic.org/diseases-conditions/stomach-cancer/symptoms-causes/syc-20352438)
Part I National Stomach Cancer Awareness Month – types and symptoms!
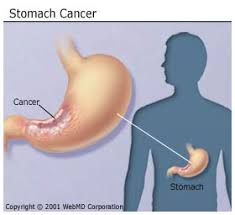
Stomach cancer (also called gastric cancer) can develop in any part of the stomach, and may spread throughout the stomach and to other organs. It may grow along the stomach wall into the esophagus or small intestine.
The cancer may also extend through the stomach wall and spread to nearby lymph nodes and organs, such as the liver, pancreas and colon. It may spread to distant organs, such as the lungs, the lymph nodes above the collarbone and to a woman’s ovaries.
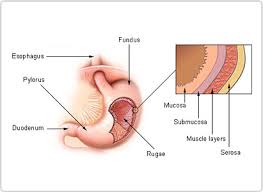
Stomach cancer happens when cells start behaving abnormally, growing and proliferating uncontrollably. The stomach, a hollow organ that collects food and breaks it down, has five different parts—from the top of the stomach, which connects to the esophagus, to the bottom of the stomach, which connects to the small intestine:
- Cardia, the area nearest to the esophagus
- Fundus, the upper stomach
- Corpus, the main body of the stomach
- Antrum, where food gets broken down by stomach acid
- Pylorus, which connects to the small intestine
There are also five layers of tissue and muscle that surround the stomach and make up the stomach wall. Going from inner to outer, the layers are:
- Mucosa
- Submucosa
- Muscularis propria
- Subserosa
- Serosa
Stomach cancer progressively spreads through these different layers. Establishing how far within the stomach wall the cancer has spread is a part of the staging process (LIKE all cancers), which determines how serious the cancer is and how best to treat it.
The mucosa layer, which produces stomach acid, is where most stomach cancers begin.
A less common type of stomach cancer is caused by gastrointestinal stromal tumors (GISTs), which start in immature cells called interstitial cells of Cajal.
Other rare stomach cancer types, such as lymphoma and neuroendocrine tumors, start in different cell types in the stomach.
Different types of stomach cancer include:
- Adenocarcinomas develop within the cells of the innermost lining of the stomach. The majority of stomach cancers are classified as adenocarcinomas.Most stomach cancer cases, about 90 percent to 95 percent, are adenocarcinomas, according to the American Cancer Society (ACS).Adenocarcinomas are broken down into two categories:
- Intestinal adenocarcinomas are usually slow-growing and more treatable. Oftentimes, these cancers may be treated with therapy drugs that are designed to target specific mutations in cancer cells. This type most often occurs in men and older adults.
- Diffuse adenocarcinomas are less common than intestinal adenocarcinomas and usually more aggressive. They tend to be faster growing, often spreading (metastasizing) to other parts of the body quickly. This type is more common at a younger age than intestinal adenocarcinomas.
- Lymphoma is a cancer of the immune system tissue that may start anywhere there are lymph tissues, including the stomach. However, lymphomas in the stomach are rare, accounting for about 4 percent of all stomach cancers. MALT (mucosa-associated lymphoid tissue) lymphoma is a type of non-Hodgkin lymphoma that typically occurs in the stomach. The cancer starts in lymph tissue that lines the stomach.
- Gastrointestinal stromal tumors, or GISTs, are a rare type of stomach cancer that starts in a special cell found in the lining of the stomach called interstitial cells of Cajal (ICCs). Under a microscope, GIST cells look similar to muscle or nerve cells. These tumors may develop throughout the digestive tract, but about 60 to 70 percent occur in the stomach. In the United States, 4,000 to 6,000 new GIST cases throughout the GI tract are diagnosed per year, according to the ACS.
- Carcinoid tumors typically start in the hormone producing cells of the stomach. These tumors usually do not spread to different organs and account for only about 3 percent of stomach cancer incidence. About 8,000 gastrointestinal carcinoid tumors are diagnosed in the United States each year, according to the ACS. Not all of these cancers start in the stomach—they may also occur in the intestines, appendix, colon and rectum.
Early stage cancers especially adenocarcinoma(s) may cause:
- Indigestion
- Bloating
- Nausea
- Poor appetite
- Heartburn
As these cancers advanced, they may cause:
- Bloody stool
- Vomiting
- Unexplained weight loss
- Belly pain
- Jaundice (yellowing of the skin and eyes)
- Difficulty swallowing
QUOTE FOR THE WEEKEND:
“An estimated 65 million people worldwide have epilepsy, and one in 26 Americans will develop epilepsy in their lifetime. Most of these people are able to control their seizures with medications, but approximately 30% to 40% have what’s called drug-resistant or medically refractory epilepsy, in which they don’t respond to standard anti-seizure medications. There are a few options available for people with drug-resistant epilepsy who need alternative RXs. The most common alternative one is epilepsy surgery, which has been performed since the 1940s. For a patient with focal epilepsy, where the seizures are being caused by one part of the brain, you try to remove the seizure focus. Somewhere between 60% and 70% of patients with drug-resistant epilepsy who have this surgery become seizure-free, which is the standard of care if the medications were not to work. Open brain surgery is effective but also carries higher risk for complications, pain and psychological impacts. Recently, minimally invasive epilepsy brain surgery has advanced quite significantly, particularly a procedure called laser ablation for patients with epilepsy. In that surgery, inserted is a small laser fiber and burn away the seizure focus in the brain but an opening up of the skull is not needed.”
UChicago Medicine (https://www.uchicagomedicine.org/forefront/neurosciences-articles/new-treatment-options-for-people-with-drug-resistant-epilepsy)
Part VI Continuation on Epilepsy Treatments if meds don’t work=Alternative Treatments!
Epilepsy is a medical disorder in which seizures can occur anytime, anywhere. An epileptic seizure is an excessive, uncontrolled burst of electrical activity from nerve cells in the brain – essentially an electrical storm. There are many types of seizures that cause symptoms ranging from lightning-fast muscle jerks lasting less than a second to full body convulsions lasting two or three minutes.
Epilepsy, if not well-controlled, can greatly worsen a person’s quality of life and can cause severe injury or death. And every person with epilepsy responds in a unique and often unpredictable way to treatment, so we need as many treatments as possible.
The medical community continually tests and approves new treatments. Here are 10 treatments, both basic and advanced, that I’ve tried to rank from least to most envasive. However, almost all treatments involve some degree of risk. Discuss your options carefully with your neurologist to pick the best treatment for you as you should for any condition.
Request an appointment to discuss your epilepsy treatment options.
1. Lifestyle changes and complementary or alternative treatments
This topic is too often neglected but can have a major, positive impact on seizure control. Though there is little evidence for the effectiveness of most complementary and alternative medications, healthy lifestyle changes can go a long way toward reducing the risk of having a seizure.
Your neurologist should address these questions with you before developing a treatment plan:
● How is your sleep quality?
● Do you have chronic anxiety, depression, or excessive stress?
● Do you take other medications that may affect your epilepsy medication or directly increase the risk you will have a seizure?
● Does your use of alcohol, caffeine, or herbal remedies affect your seizure control?
The complementary and alternative therapies below can be added to your treatment plan. Because there is not a lot of medical research on their effectiveness for epilepsy, it’s important to discuss each treatment with your neurologist:
● Acupuncture
● Aerobic exercise
● Biofeedback (training to voluntarily control seizures)
● Meditation
● Yoga
I don’t hesitate to recommend aerobic exercise and meditation for all my patients — both usually are win-win treatments! It’s rare that doctors would recommend only lifestyle changes or complementary/alternative treatments for epilepsy; however, these might work sometimes.
I recently had a patient who, after experiencing a single seizure, was diagnosed with a genetic form of epilepsy. She was a student whose seizure occurred after several nights of staying up late studying and
drinking alcohol excessively. It was clear that her risk of having a seizure was higher than normal. However, it was possible that in the setting of a healthier lifestyle this might not occur. After discussing options, she and her parents decided to delay taking medication and first try to make lifestyle changes, including getting more sleep and minimizing or avoiding alcohol.
There is not much evidence that herbal remedies help with epilepsy. But medical marijuana, which is number four on this list, proves that plants have chemicals that can stop epileptic seizures (see below). At this time, we know of no other natural herb that helps with seizures. In fact, some herbs, such as the Chinese herb ma huang, can trigger or worsen seizures. Ma huang is a natural ephedra, which is similar to a stimulant hormone in our bodies. Stimulants tend to worsen seizures, so doctors are hesitant to recommend any herbal remedies at this time.
2. Diet
For many years, a special diet has been used to control certain types of epilepsy. One in particular – the ketogenic diet – gained public attention with the 1997 movie “First Do No Harm.” In this film, which is based on a true story, Meryl Streep plays the mother of a son whose epilepsy fails to respond to conventional treatments, including epilepsy surgery. She takes him to Johns Hopkins Medical Center, which pioneered the use of the ketogenic diet and demonstrated its effectiveness. Her son responded wonderfully to the diet and became seizure-free.
The ketogenic diet is strict. It severely limits carbohydrates and maximizes fats and proteins. This low-carbohydrate diet triggers ketosis, an alternate metabolic pathway in the body that somehow works against seizures. Variations in the amount of fats and proteins relative to the amount of carbohydrates are allowed. One such variation is the Modified Atkins Diet.
The ketogenic diet is challenging and is used mostly for children. A few studies have shown its effectiveness in adults, but, as one might expect, it’s difficult for most adults to maintain such a strict diet. Choosing this type of therapy requires support from experienced nurses, dietitians, and physicians who can help guide food and drink choices.
Although it may seem like the ketogenic diet has been recently created, it’s not a newly discovered way of eating. In fact, the ketogenic diet was first put into practice in the 1920s as a treatment for people with epilepsy after research demonstrated that fasting reduced seizure activity.
What exactly is the ketogenic diet? The ketogenic diet is an eating pattern that includes high amounts of fat, low to moderate amounts of protein, and very little carbohydrates. The keto diet is typically rich in foods like butter, cheese, eggs, meat, nuts, oils, seafood, and seeds. It does not allow much, if any, room for fruits, vegetables, grains, potatoes, sweets, or other carbohydrate-rich foods.
Although there are variations to the ketogenic diet, they all share a primary objective of restricting carbohydrate intake. A typical ketogenic eating plan aims for about five percent of calories from carbohydrates, 20 percent from protein, and 75 percent from dietary fats. On a 2,000-calorie-per-day ketogenic diet, this equates to about 100 calories (25 grams) of carbohydrates, 400 calories (100 grams) of protein, and 1,500 calories (167 grams) of dietary fat.
4. Medical marijuana
Medical marijuana is a term that now refers to one of more than 80 chemical compounds found in the cannabis plant – cannabidiol oil or CBD oil. This treatment came to national attention in 2013 with the story of Charlotte, a child living with Dravet syndrome in Colorado. Dravet syndrome is a severe form of genetic epilepsy, and Charlotte was having many seizures every day. CBD oil helped effectively manage Charlotte’s seizures, which has led to formal clinical studies that have proved its effectiveness.
CBD oil lacks the compound tetrahydrocannabinol (THC), so it does not appear to cause any significant mood-altering effects (“getting high”), at least compared to smoking the marijuana leaves. As of May 2018, there have been two major, scientifically rigorous clinical studies that have shown that Epidiolex, a form of CBD oil pending FDA approval, is relatively safe and effective in Dravet Syndrome and the Lennox-Gastaut Syndrome. It has been approved by the scientific advisory committee of the FDA, but final approval is pending. At this time, CBD oil is expensive. We need more research to assess its efficacy for other types of epilepsy and its possible long-term effects.
5. Medication trials
At any time, a patient may be invited to participate in a trial of an experimental medication. Since about 1993, this is how all medications have received FDA approval. Often, patients are invited to join a trial after they have failed a number of other FDA-approved medications.
The advantages of participating in a clinical trial include:
● Access to new medication
● Close support and follow-up with the epilepsy team
● The opportunity to help medical researchers develop new treatments
The goal of medication clinical trials is to make sure the drugs are safe and effective. Clinical trials are experimental studies, so there is some risk involved with participating. However, clinical research teams follow extremely strict federal, state, and hospital guidelines to ensure that the risks are minimized.
6. Extracranial neurostimulators
Neurostimulators deliver electrical stimulation to the brain. Some stimulate nerves that are not in the brain, which then transfer the electrical stimulation to the brain; we refer to these as extracranial stimulators.
The first and most common stimulation of this type is the vagus nerve stimulation (VNS), in which an electrode is wrapped around the vagus nerve on the left side of the neck and a computer battery is implanted under the skin below the collar bone. We start with the stimulator set to deliver a 30-second electrical impulse every five minutes. Each patient has a magnet that activates the device immediately and at a higher intensity if a seizure occurs. Newer versions of the VNS also can trigger a stimulus when the patient’s heartbeat goes too fast, which often happens with an epileptic seizure.
Another type of neurostimulation currently being investigated is external trigeminal nerve stimulation. This therapy stimulates a nerve on the face and does not require surgery.
7. Immunotherapy
Occasionally, epilepsy is caused by the patient’s immune system attacking the brain. Autoimmune epilepsy is a relatively recently recognized cause of epilepsy that cannot be controlled with anti-seizure medications alone.
Typically, the patient produces antibodies that attack parts of the brain, and these antibodies can be identified with a blood test. Some patients have autoimmune epilepsy, but no antibody can be identified at this time.
Treatment options include:
● High-dose steroids
● Administering a collection of human antibodies through the veins
● Plasma exchange to filter the blood of disease-causing antibodies
● Other medications that suppress the overly active immune system
8. Responsive neurostimulation (RNS®)
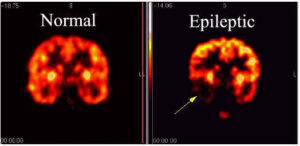
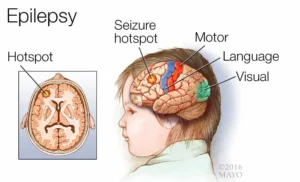
If epileptic seizures are coming from one specific region of the brain, and they cannot be stopped with medications or other therapies we have discussed, the patient can be a candidate for intracranial neurostimulation.
This first requires identifying exactly where the seizures are coming from – the seizure focus. Sometimes this can be done by recording the patient’s seizures with electrodes on the scalp using video-EEG. Often, however, we need to use intracranial electrodes to confidently determine the location of the seizure focus.
If the patient does not want surgery, if there is more than one seizure focus, or if it would be too risky to remove the seizure focus, the patient can choose intracranial automatic neurostimulation, a system developed by NeuroPace Inc.
The neurosurgeon inserts electrodes within one or more brain regions where seizures start. The electrodes detect the onset of a seizure and trigger an immediate electrical impulse in the seizure focus, which we hope will stop the seizure. It’s like fighting fire with fire. This is similar to automatic heart defibrillators for patients with potentially fatal heart arrhythmias. The main risks are scalp infections and bleeding when the electrodes are inserted.
9. Deep brain stimulation (DBS)
DBS is similar to RNS®, but the electrodes are implanted in a deep brain region called the thalamus. It has been shown effective for focal seizures, which start consistently in one specific area of the brain. Unlike RNS, it stimulates on a regular basis rather than triggering only when a seizure starts. The stimulation is directly within the brain. Also unlike RNS, it is not necessary to localize where the seizure starts. As of May 2018, the FDA has approved DBS for patients with focal epilepsy.
10. Brain surgery
Brain surgery to remove the seizure focus is the most effective method to completely stop seizures. First, we must find the seizure focus and make sure it can be safely removed. This always involves a stay in the epilepsy monitoring unit to record seizures with simultaneous video and EEG.
Sometimes the seizure focus cannot be determined with electrodes on the scalp, and we need to put electrodes directly within the brain. This is called intracranial EEG. The most common location in the brain for epilepsy surgery is the temporal lobe. About 60 percent to 80 percent of patients become seizure-free with this type of surgery.
A new technique is laser surgery, which involves destroying the seizure focus with heat rather than removing it. This technique is especially useful for seizures coming from deep structures in the brain and is much less invasive. Other types of surgeries include “disconnections,” in which the seizure focus is not removed but rather is prevented surgically from spreading to other areas of the brain.
The goal is to stop all seizures and to avoid any side effects that would affect the quality or safety of the patient’s life. The process sometimes can be a struggle, but we will never give up. By the time you read this, I hope there will be more treatments approved and in testing. Be sure to have a detailed discussion with your neurologist about an up-to-date treatment plan that works best for you.
QUOTE FOR FRIDAY:
“Epilepsy is sometimes referred to as a long-term condition, as people often live with it for many years, or for life. Although generally epilepsy cannot be ‘cured’, for most people, seizures can be ‘controlled’ (stopped) so that epilepsy has little or no impact on their lives. So treatment is often about managing seizures in the long-term.
Most people with epilepsy take anti-seizure medication (ASM), previously known as anti-epileptic drugs or AEDs, to stop their seizures from happening. However, there are other treatment options for people whose seizures are not controlled by ASM.”
Epilepsy Society (https://epilepsysociety.org.uk/about-epilepsy/treatment)