Complications can include:
-Diabetes (High or Low blood glucose levels)
-Enlargement of pituitary tumor and other complications from the tumor growth
-Fractures due to osteoporosis which are common in older people
-High blood pressure which could be life threatening
-Kidney stones from the increase in cortisol and other chemicals filtered through the kidneys
-Serious infections which could lead to further secondary infections
How Cushing’s syndrome is diagnosed and treated?
Diagnosis is established on a survey of the patient’s medical history including somatic examination and laboratory tests.
Frequently x-ray exams of the adrenal or pituitary glands are beneficial for locating tumors. These tests assist to find out if excess levels of cortisol are exhibited and why.
Radiologic imaging: direct visualization of the endocrine glands. Imaging tests reveal the size and shape of the pituitary and adrenal glands and help determine if a tumor is present. The most common imaging tests are the computerized tomography (CT) scan and magnetic resonance imaging (MRI). A CT scan produces a series of x-ray pictures giving a cross-sectional image of a body part. MRI also produces images of internal organs but without exposing patients to ionizing radiation.
Imaging procedures are used to find a tumor after a diagnosis has been made. Imaging is not used to make the diagnosis of Cushing’s syndrome because benign tumors are commonly found in the pituitary and adrenal glands. These tumors, sometimes called incidentalomas, do not produce hormones in quantities that are harmful. They are not removed unless blood tests show they are a cause of symptoms or they are unusually large. Conversely, pituitary tumors may not be detectable by imaging in almost half of people who ultimately need pituitary surgery for Cushing’s syndrome.
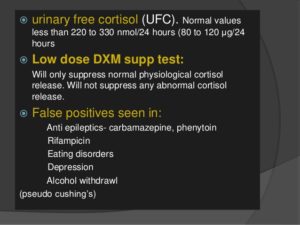
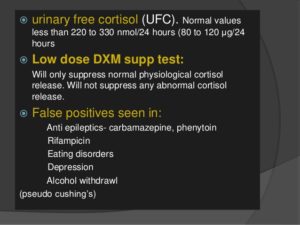
24-hour urinary free cortisol level. In this test, a person’s urine is collected several times over a 24-hour period and tested for cortisol. Levels higher than 50 to 100 micrograms a day for an adult suggest Cushing’s syndrome. Low-dose dexamethasone suppression test (LDDST). In the LDDST, a person is given a low dose of dexamethasone, a synthetic glucocorticoid, by mouth every 6 hours for 2 days. Urine is collected before dexamethasone is administered and several times on each day of the test. A modified LDDST uses a onetime overnight dose.
The normal upper limit varies in different laboratories, depending on which measurement technique is used.
Midnight plasma cortisol and late-night salivary cortisol measurements. The midnight plasma cortisol test measures cortisol concentrations in the blood.
Dexamethasone-corticotropin-releasing hormone (CRH) test. Some people have high cortisol levels but do not develop the progressive effects of Cushing’s syndrome, such as muscle weakness, fractures, and thinning of the skin. These people may have pseudo-Cushing’s syndrome, a condition sometimes found in people who have depression or anxiety disorders, drink excess alcohol, have poorly controlled diabetes, or are severely obese. Pseudo-Cushing’s does not have the same long-term effects on health as Cushing’s syndrome and does not require treatment directed at the endocrine glands.
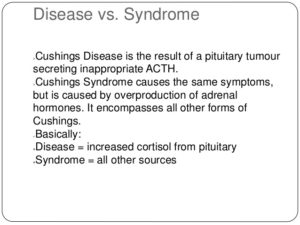
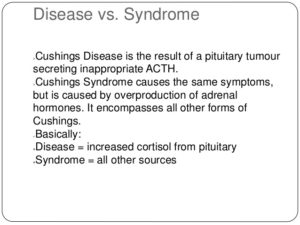
Treatment of Cushings Syndrome:
Treatment of cushings syndrome is by castigation of the under lying cause. Treatments for Cushing’s syndrome are contrived to pass your body’s cortisol production to normal. By indurate, or even distinctly lowering cortisol levels, you’ll feel evident improvements in your signs and symptoms. Left untreated, however, Cushing’s syndrome can finally induce to death. The treatment choice depend on the cause. For example:
*If a tumour in an adrenal gland is the reason, an operation to withdraw it will cure the condition.
*For adrenal hyperplasia, both adrenal glands may require to be withdraw. You will then require to take lifelong replacement therapy of several adrenal hormones.
*Other tumours in the body that produce ‘ectopic’ ACTH may be able to be removed, depending on the kind of tumour, where it is, etc.
*Medication to block the production or consequence of cortisol may be a choice.
Ending line treatments for Cushing syndrome are designed to lower the high level of cortisol in your body. The best treatment for you depends on the cause of the syndrome. Treatment options include:
- Reducing corticosteroid use. If the cause of Cushing syndrome is long-term use of corticosteroid medications, your doctor may be able to keep your Cushing signs and symptoms under control by reducing the dosage of the drug over a period of time, while still adequately managing your asthma, arthritis or other condition. For many of these medical problems, your doctor can prescribe noncorticosteroid drugs, which will allow him or her to reduce the dosage or eliminate the use of corticosteroids altogether.
Don’t reduce the dose of corticosteroid drugs or stop taking them on your own. Do so only under your doctor’s supervision.
Abruptly discontinuing these medications could lead to deficient cortisol levels. Slowly tapering off corticosteroid drugs allows your body to resume normal cortisol production.
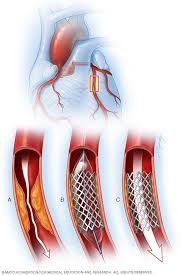
- If the cause of Cushing syndrome is a tumor, your doctor may recommend complete surgical removal. Pituitary tumors are typically removed by a neurosurgeon, who may perform the procedure through your nose. If a tumor is present in the adrenal glands, lungs or pancreas, the surgeon can remove it through a standard operation or in some cases by using minimally invasive surgical techniques, with smaller incisions.
After the operation, you’ll need to take cortisol replacement medications to provide your body with the correct amount of cortisol. In most cases, you’ll eventually experience a return of normal adrenal hormone production, and your doctor can taper off the replacement drugs.
However, this process can take up to a year or longer. In some instances, people with Cushing syndrome never experience a resumption of normal adrenal function; they then need lifelong replacement therapy.
- Radiation therapy. If the surgeon can’t totally remove a pituitary tumor, he or she will usually prescribe radiation therapy to be used in conjunction with the operation. Additionally, radiation may be used for people who aren’t suitable candidates for surgery.
Radiation can be given in small doses over a six-week period, or with a technique called stereotactic radiosurgery (Gamma Knife surgery). In the latter procedure, administered as a single treatment, a large dose of radiation is delivered to the tumor, and the radiation exposure to surrounding tissues is minimized.
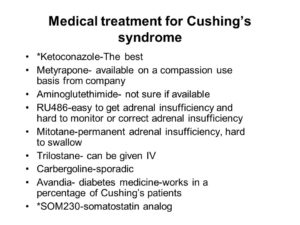
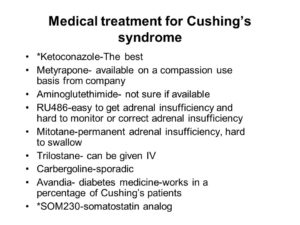
- Medications can be used to control cortisol production when surgery and radiation don’t work. Medications may also be used before surgery in people who have become very sick with Cushing syndrome. Doctors may recommend drug therapy before surgery to improve signs and symptoms and minimize surgical risk.
Medications to control excessive production of cortisol at the adrenal gland include ketoconazole (Nizoral), mitotane (Lysodren) and metyrapone (Metopirone).
Mifepristone (Korlym) is approved for people with Cushing syndrome who have type 2 diabetes or glucose intolerance. Mifepristone does not decrease cortisol production, but it blocks the effect of cortisol on your tissues.
Side effects from these medications may include fatigue, nausea, vomiting, headaches, muscle aches, high blood pressure, low potassium and swelling. Some have more serious side effects, such as neurological side effects and liver toxicity.
The newest medication for Cushing’s is pasireotide (Signifor), and it works by decreasing ACTH production from a pituitary tumor. This medication is given as an injection twice daily. It’s recommended if pituitary surgery is unsuccessful or cannot be done.
Side effects are fairly common, and may include diarrhea, nausea, high blood sugar, headache, abdominal pain and fatigue.
In some cases, the tumor or its treatment will cause other hormones produced by the pituitary or adrenal gland to become deficient and your doctor will recommend hormone replacement medications.
If none of these treatment options are appropriate or effective, your doctor may recommend surgical removal of your adrenal glands (bilateral adrenalectomy). This procedure will cure excess production of cortisol, but will require lifelong replacement medications.
Complications are rare but include:
Bruising on your thigh
Ear pain during the procedure
Very rarely, neurological problems