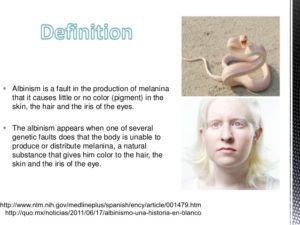
The word “albinism” refers to a group of inherited conditions. People with albinism have little or no pigment in their eyes, skin, or hair. They have inherited altered genes that do not make the usual amounts of a pigment called melanin. One person in 17,000 in the U.S.A. has some type of albinism. Albinism affects people from all races. Most children with albinism are born to parents who have normal hair and eye color for their ethnic backgrounds. Sometimes people do not recognize that they have albinism. A common myth is that people with albinism have red eyes. In fact there are different types of albinism and the amount of pigment in the eyes varies. Although some individuals with albinism have reddish or violet eyes, most have blue eyes. Some have hazel or brown eyes. However, all forms of albinism are associated with vision problems.
Vision Problems
People with albinism always have problems with vision (not correctable with eyeglasses) and many have low vision. The degree of vision impairment varies with the different types of albinism and many people with albinism are “legally blind,” but most use their vision for many tasks including reading and do not use Braille. Some people with albinism have sufficient vision to drive a car. Vision problems in albinism result from abnormal development of the retina and abnormal patterns of nerve connections between the eye and the brain. It is the presence of these eye problems that defines the diagnosis of albinism. Therefore the main test for albinism is simply an eye examination.
Skin Problems
While most people with albinism are fair in complexion, skin or hair color is not diagnostic of albinism. People with many types of albinism need to take precautions to avoid damage to the skin caused by the sun such as wearing sunscreen lotions, hats and sun-protective clothing.
Types of Albinism
While most people with albinism have very light skin and hair, not all do. Oculocutaneous (pronounced ock-you-low-kew-TAIN-ee-us) albinism (OCA) involves the eyes, hair and skin. Ocular albinism (OA), which is much less common, involves primarily the eyes, while skin and hair may appear similar or slightly lighter than that of other family members.
Over the years, researchers have used various systems for classifying oculocutaneous albinism. In general, these systems contrasted types of albinism having almost no pigmentation with types having slight pigmentation. In less pigmented types of albinism, hair and skin are cream-colored and vision is often in the range of 20/200. In types with slight pigmentation, hair appears more yellow or red-tinged and vision may be better. Early descriptions of albinism called these main categories of albinism “complete” and “incomplete” albinism. Later researchers used a test that involved plucking a hair root and seeing if it would make pigment in a test tube. This test separated “ty-neg” (no pigment) from “ty-pos” (some pigment). Further research showed that this test was inconsistent and added little information to the clinical exam.
Recent research has used analysis of DNA, the chemical that encodes genetic information, to arrive at a more precise classification system for albinism. Four forms of OCA are now recognized – OCA1, OCA2, OCA3 and OCA4; some are further divided into subtypes.
- Oculocutaneous albinism type 1 (OCA1 or tyrosinase-related albinism) results from a genetic defect in an enzyme called tyrosinase (hence ‘ty’ above). This enzyme helps the body to change the amino acid tyrosine into pigment. (An amino acid is a “building block” of protein.) There are two subtypes of OCA1. In OCA1A, the enzyme is inactive and no melanin is produced, leading to white hair and very light skin. In OCA1B, the enzyme is minimally active and a small amount of melanin is produced, leading to hair that may darken to blond, yellow/orange or even light brown, as well as slightly more pigment in the skin.
- Oculocutaneous albinism type 2 (OCA2 or P gene albinism) results from a genetic defect in the P protein that helps the tyrosinase enzyme to function. Individuals with OCA2 make a minimal amount of melanin pigment and can have hair color ranging from very light blond to brown.
- Oculocutaneous albinism type 3 (OCA3) is rarely described and results from a genetic defect in TYRP1, a protein related to tyrosinase. Individuals with OCA3 can have substantial pigment.
- Oculocutaneous albinism type 4 (OCA4) results from a genetic defect in the SLC45A2 protein that helps the tyrosinase enzyme to function. Individuals with OCA4 make a minimal amount of melanin pigment similar to persons with OCA2.
Researchers have also identified several other genes that result in albinism with other features. One group of these includes at least eight genes leading to Hermansky-Pudlak Syndrome (HPS). In addition to albinism, HPS is associated with bleeding problems and bruising. Some forms are also associated with lung and bowel disease. HPS is a less common form of albinism but should be suspected if a person with albinism shows unusual bruising or bleeding.
Genetics of Albinism
The genes for OCA are located on “autosomal” chromosomes. Autosomes are the chromosomes that contain genes for our general body characteristics, contrasted to the sex chromosomes. We normally have two copies of these chromosomes and the genes on them – one inherited from our father, the other inherited from our mother. Neither of these gene copies is functional in people with albinism. However, albinism is a “recessive trait”, so even if only one of the two copies of the OCA gene is functional, a person can make pigment, but will carry the albinism trait. Both parents must carry a defective OCA gene to have a child with albinism. When both parents carry the defective gene (and neither parent has albinism) there is a one in four chance at each pregnancy that the baby will be born with albinism. This type of inheritance is called “autosomal recessive” inheritance.
Ocular albinism (OA1) is caused by a genetic defect of the GPR143 gene that plays a signaling role that is especially important to pigmentation in the eye. OA1 follows a simpler pattern of inheritance because the gene for OA1 is on the X chromosome. Females have two copies of the X chromosome while males have only one copy (and a Y chromosome that makes them male). To have ocular albinism, a male only needs to inherit one defective copy of the gene for ocular albinism from his carrier mother. Therefore almost all of the people with OA1 are males. Indeed, parents should be suspicious if a female child is said to have ocular albinism.
For couples who have not had a child with albinism, there is no simple test to determine whether a person carries a defective gene for albinism. Researchers have analyzed the DNA of many people with albinism and found the changes that cause albinism, but these changes are not always in exactly the same place, even for a given type of albinism. Moreover, many of the tests do not find all possible changes. Therefore, the tests for the defective gene may be inconclusive.
If parents have had a child with albinism previously, and if that affected child has had a confirmed diagnosis by DNA analysis, there is a way to test in subsequent pregnancies to see if the fetus has albinism. The test uses either amniocentesis (placing a needle into the uterus to draw off fluid) or chorionic villous sampling (CVS). Cells in the fluid are examined to see if they have an albinism gene from each parent.
For specific information and genetic testing, seek the advice of a qualified geneticist or genetic counselor. The American College of Medical Genetics and the National Society of Genetic Counselors maintain a referral list. Those considering prenatal testing should be made aware that people with albinism usually adapt quite well to their disabilities and lead very fulfilling lives.
Vision Rehabilitation
Eye problems in albinism result from abnormal development of the eye because of lack of pigment and often include:
- Nystagmus: regular horizontal back and forth movement of the eyes
- Strabismus: muscle imbalance of the eyes, “crossed eyes” (esotropia), “lazy eye” or an eye that deviates out (exotropia)
- Photophobia: sensitivity to bright light and glare
- People with albinism may be either far-sighted or near-sighted and usually have astigmatism
- Foveal hypoplasia: the retina, the surface inside the eye that receives light, does not develop normally before birth and in infancy
- Optic nerve misrouting: the nerve signals from the retina to the brain do not follow the usual nerve routes
- The iris, the colored area in the center of the eye, has little to no pigment to screen out stray light coming into the eye. (Light normally enters the eye only through the pupil, the dark opening in the center of the iris, but in albinism light can pass through the iris as well.)
For the most part, treatment of the eye conditions consists of visual rehabilitation. Surgery to correct strabismus may improve the appearance of the eyes. However, since surgery will not correct the misrouting of nerves from the eyes to the brain, surgery will not improve eyesight or fine binocular vision. In the case of esotropia or “crossed eyes,” surgery may help vision by expanding the visual field (the area that the eyes can see while looking at one point).
People with albinism are sensitive to glare, but they do not prefer to be in the dark, and they need light to see just like anyone else. Sunglasses or tinted contact lenses help outdoors. Indoors, it is important to place lights for reading or close work over a shoulder rather than in front.
Various optical aids are helpful to people with albinism and the choice of an optical aid depends on how a person uses his or her eyes in jobs, hobbies, or other usual activities. Some people do well using bifocals which have a strong reading lens, prescription reading glasses, or contact lenses. Others use hand-held magnifiers or special small telescopes and some prefer to use screen magnification products on computers.
Some people with albinism use bioptics, glasses which have small telescopes mounted on, in, or behind their regular lenses, so that one can look through either the regular lens or the telescope. Newer designs of bioptics use smaller light-weight lenses. Some states allow the use of bioptic telescopes for driving.
Optometrists or ophthalmologists who are experienced in working with low vision patients can recommend various optical aids. Clinics should provide aids on trial loan and provide instruction in their use. The American Foundation for the Blind maintains a directory of low vision clinics. In Canada, support is available from the Canadian National Institute for the Blind.
Medical Problems
In the United States, most people with albinism live normal life spans and have the same types of general medical problems as the rest of the population. The lives of people with Hermansky-Pudlak Syndrome can be shortened by lung disease or other problems. Other conditions include Chediak-Higashi and Griscelli Syndrome.
In tropical countries, those who do not use skin protection may develop life-threatening skin cancers. If they use appropriate skin protection, such as sunscreen lotions rated 20 SPF or higher and opaque clothing, people with albinism can enjoy outdoor activities even in summer.
People with albinism are at risk of isolation because the condition is often misunderstood. Social stigmatization can occur, especially within communities of color, where the race or paternity of a person with albinism may be questioned. Families and schools must make an effort not to exclude children with albinism from group activities. Contact with others with albinism or who have albinism in their families or communities is most helpful. NOAH can provide the names of contacts in many regions of the country.
Funding for the development and original printing of this information Bulletin was provided by the Innovating Worthy Projects Foundation of Somers Point, New Jersey. NOAH gratefully acknowledges their assistance. Revised 2007 by Rick Thompson, O.D., F.A.A.O. NOAH Board of Scientific Advisors, Kelsey Thompson, M.S., C.R.C., Chair, NOAH Editorial Committee.
Resources
Hermansky-Pudlak Syndrome Network
A NOAH affiliate providing information and support to individuals and families with HPS
One South Road
Oyster Bay, NY 11771-1905
Phone: 800-789-9HPS
Web: www.hpsnetwork.org
Positive Exposure
A nonprofit organization offering innovative photographic exhibits, challenging the stigma associated with difference and celebrating the richness of genetic variation.
43 E. 20th St., 6th Floor
New York, NY 10003
Phone: 212-420-1931
Web: www.positiveexposure.org
American Foundation for the Blind (AFB)
Provides information about programs and clinics for people with impaired vision throughout the United States
11 Penn Plaza, Suite 300
New York, NY 10001
Phone: 800-AFB-LIND
Web:www.afb.org