THE KEY is to not allowing a Health Acquired Infection-HAI to even occur; this is through PREVENTION!
To reach this key is to understand exactly what a HAI is and how they work in spreading. If you didn’t get a chance to read Tues. Part 1, Wed. Part 2 and Thurs. Part 3 articles do that first to learn what HAIs actually are. The public has to get focused.
Prevention with the most common HAI is UTIs, the CDC recommends healthcare workers to do the following:
- Insert urinary catheters only for the appropriate indications & minimize their use in those at high risk of UTIs, especially the elderly, women, & immunocompromised patients.
- Leave catheters in place only for as long as needed. Remove catheters on postoperative patients as soon as possible, preferably within 24 hours unless there are appropriate indications for continued use.
- Avoid use of urinary catheters in patients and nursing home residents for the management of incontinence. It is better to be do 2hr checks on the patient&do clean up immediately.
- Ensure that only properly trained persons insert and maintain catheters.
- Insert catheters using aseptic technique and sterile equipment. Use proper CDC hand hygiene and standard or appropriate isolation precautions (see discussion of these topics later in this course) when inserting or handling catheters. Perform hand hygiene immediately before and after insertion or any manipulation of the catheter site or device.
- Maintain a closed drainage system with unobstructed urine flow. Urinary catheter systems with preconnected, sealed catheter-tubing junctions are suggested for use.
- Do not clamp indwelling catheters prior to removal and do not change indwelling catheters or drainage bags at routine intervals. Catheters and drainage bags should be changed based on clinical indications, such as infection, obstruction, or when the closed system is compromised.
- Any visitors should wash hands before entering and upon leaving following with antiseptic cleaner, like Purell. If the pt is on any isolation a sheet taped to the door will show all instructions of what the visitor should do before entering the room and if not sure the visitor can always ask the RN or staff.Prevention is key to eliminating central line acquired bloodstream infections in healthcare facilities. The CDC recommends healthcare professionals follow these guidelines to reduce CLABSIs in the workplace:
- Prevention of an infection regarding female as a gender there is nothing you can do about that or the anatomy of the urethra. After having sex there is something you can do in attempting prevention of a UTI. A women can clean the perineal/vaginal area right after the activity to decrease the chance of an infection from occurring through entering her urethra or even or vagina, with thorough drying. Remember water attracts bacteria. Staff shold choose proper central line insertion sites to minimize infections and mechanical complications. Avoid the femoral site in adult patients.
- Staff follow proper insertion practices, including complying with hand hygiene recommendations; using maximum sterile barrier precautions, performing adequate skin antisepsis with > 0.5% chlorhexidine with alcohol; and covering the site with sterile gauze or sterile, transparent, semipermeable dressings.
- Staff accessing the line, scrub the hub/port with an appropriate antiseptic (e.g., chlorhexidine, povidone iodine, an iodophor, or 70% alcohol) and access lines only with sterile devices.
- Replace dressings that are wet, soiled, or dislodged. When changing dressings, use aseptic technique, including clean and sterile gloves, as per facility policy.
- Staff perform daily audits to determine if a central line is still needed, and remove unnecessary central lines.
- Any visitors should wash hands before entering and upon leaving. If the pt is on any isolation a sheet taped to the door will show all instructions of what the visitor should do before entering the room and if not sure the visitor can always ask the RN or staff.
- Prior to Surgery
- The key to prevention with surgery sites getting infected is the following:
- Administer prophylactic antibiotics in accordance with evidence-based standards and guidelines 1 hour before surgery. This will help prevent an infection from occurring.
- Whenever possible, identify and treat remote infections before elective surgery, or postpone surgery until the infection has resolved.
- Prep skin using an appropriate antiseptic agent and proper technique. Do not remove hair at the operative site unless it will interfere with the operation. If hair must be removed, razors should not be used.
- For colorectal surgery patients, mechanically prepare the colon (enemas, cathartic agents).
- During Surgery the following takes place:
- Keep operating room doors closed during surgery except as needed for passage of equipment, personnel, and the patient.
- Consider re-dosing antibiotics at the 3-hour interval in procedures lasting longer than 3 hours and adjust the antimicrobial prophylaxis dose for patients with a body mass index greater than 30.
- Consider using at least 50% fraction of inspired oxygen intra-operatively and immediately postoperatively in select procedures.
- After Surgery
- Protect the primary closure incision with a sterile dressing for 24–48 hours post op.
- Maintain immediate postoperative normothermia.
- For cardiac surgeries, control blood glucose levels during the immediate postoperative period. Glucose level should be measured at 6:00 a.m. on postop day 1 and day 2 (procedure day is postop day 0). Postop glucose level should be maintained at < 200mg/dL.
- Discontinue antibiotics according to evidence-based standards and guidelines (within 24 hours after surgery end time, or 48 hours for cardiac surgeries).
- Any visitors should wash hands before entering and upon leaving. If the pt is on any isolation a sheet taped to the door will show all instructions of what the visitor should do before entering the room and if not sure the visitor can always ask the RN or staff.
- Patients with MRSA, VRE, and C-DIFF HCIs are placed in single contact isolation rooms, or, if a single room is not available, cohort patients put the patients in the same room or in the same patient care area with the same HCI (Ex. Both patients with VRE in their urine). Treatment by healthcare workers for patients with MRSA, VRE, and C-DIFF infections is to use proper standard isolation techniques plus contact isolation techniques to prevent spreading of the HCI to anyone out of the room or to them-selves. Anyone visitor the patient with MRSA, VRE or C-DIFF would be educated on how to prevent spreading these HCIs out of the room with protecting themselves from getting the infection.
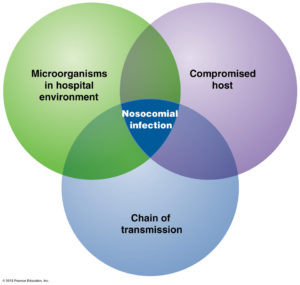
- Some bacteria does not need a living host to survive. Microbes such as MRSA, vancomycin-resistant enterococci (VRE), and C. difficile can survive for long periods on environmental surfaces, such as bedrails and phones. After being contaminated, these environmental surfaces become the source of infection. A clean healthcare environment is essential for prevention of infection from these organisms.
- The other way in prevention of these HCIs are through cleaning and disinfection of the patient environment. This includes high touch surfaces, such as bedrails, carts, toilets, and doorknobs, as well as general housekeeping surfaces, such as floors, walls, and blinds. Proper disinfection and sterilization of medical and surgical instruments and devices are also vital in the prevention of HAIs.
- The Joint Commission includes infection prevention as one of its National Patient Safety Goals in hospitals, behavioral care facilities, and ambulatory care facilities, as well as home health care. Specifically, the Joint Commission emphasizes handwashing as key to infection prevention. Although hand hygiene and transmission precautions are routine in healthcare facilities, a review of evidence-based practice can remind healthcare professionals of the process of and rationale for these procedures.
- Handwashing is the single most effective way to prevent the transmission of infection.
- The public must get involved with medical staff to stay on top of prevention with HAIs. This is to allow HAIs to go on a continual reduction. This will only occur if both staff of a health care facility get involved with the public. Having everyone nationally in all communities take part will only happen if increased health awareness is provided, which in the end will help decrease infection. This will indirectly put a reduction on our medical debt, which will take time. Our medical technology has taken us so far in learning and treating infection compared to 100 years ago or less; but we need the public to get more focused on how to prevent HAIs as well. We can’t leave it up to the health care facilities staff to only take action to prevent HAIs. The public needs to take part in this now. Broadening the public’s knowledge will help prevent people from getting a HAI when admitted to the hospital or going to any type of medical facility for care. It also will get the public more focused on HAIs allowing the family with the patient to take more action in prevention of HAIs (The key).
- We the people in our society are responsible in reaching the goal for better health. The medical staff, who is already carrying out infection control measures, with the public’s help through increased knowledge on HAIs will only increase the chance of continued reduction in infections, to possibly minimal infections one day, in all types of hospitals or health care facilities. We all must get focused!