1-C-DIFF or C-difficile, know as Clostridium difficile infection (CDI), or Clostridium difficile–associated disease (CDAD), which is an infection of the intestines caused by the anaerobic, spore-forming, gram-positive bacillus C. difficile. This microbe was first identified in 1935 when it was isolated from the stools of neonates. C. difficile produces heat-resistant spores that can remain viable on fomites in the environment for years, becoming a source of outbreaks in healthcare facilities. This bacillus also produces two types of toxins: Toxin A (an enterotoxin) and Toxin B (a cytotoxin). These toxins are responsible for the inflammatory responses of the colon, which results in loss of epithelial integrity and the production of watery diarrhea. C. difficile is the most common cause of antibiotic-associated diarrhea and pseudomembranous colitis and has proved extremely difficult to control due to new, more resistant strains.
- difficile is found in the intestinal tract of up to 70% of healthy infants, 1–3% of healthy adults, and in higher rates (up to 20%) in persons on antibiotic therapy. Prevalence, severity, colectomy rates, and mortality rates due to C. difficile have all risen in the past two decades, proving that this microbe has become an extremely virulent superbug that is both persistent and difficult to treat. Surveillance data from the CDC show that between 2000 and 2007 mortality from C. difficile increased by 400% due to a more virulent strain of this organism.
Studies of hospital-acquired CDI have shown that the infection is independently associated with increased risk of in-hospital death: For every 10 hospital patients who acquire a CDI, 1 patient died. Data from the CDC show that C. difficile is responsible for 337,000 infections and 14,000 deaths in the United States each year.
The greatest risk factor for CDI is the use of antibiotics, such as cephlasporins, clindamycin, or the penicillins, because these antibiotics kill the normal flora of the colon, causing overgrowth of C. difficile. Risk is increased for those taking multiple antimicrobials and those who take antimicrobials for longer time periods. Other risk factors for CDI include advanced age. Although almost half of the infections occur in persons younger than 65, most CDI-related deaths occur in the elderly. People with HIV infection, compromised immune systems, and compromised physical status are also at increased risk for CDI. Hospital admission increases one’s chance of acquiring CDI, as does gastrointestinal surgery.
Transmission of CDI occurs by the fecal-oral route.
The time between exposure to C. difficile and infection is 2 to 3 days. Symptoms of CDI vary greatly, ranging from asymptomatic to mild (fever, malaise, and gastrointestinal symptoms, including abdominal pain and cramps, and mild to moderate foul-smelling diarrhea that is rarely bloody) to extremely severe toxic megacolon, septic shock, and even death. Complications of C. difficile include pseudomembranous colitis or fulminant colitis.
Diagnosis is based on clinical history (antibiotic use in the previous 2 months, diarrhea after 72 or more hours of hospitalization), and presence of C. difficile in the stool. Stool culture is the most sensitive test and is often used for diagnosis in the hospital setting. Colonoscopy revealing histopathology with pseudomembranous colitis is also diagnostic but not necessary in most cases.
Treatment for CDI begins with discontinuation of the antibiotic causing the infection. In many cases, this step is the only necessary treatment since normal flora can reestablish in the colon. If mild to moderate diarrhea persists, patients can be treated with either metronidazole or vancomycin. In cases of severe diarrhea, vancomycin is the drug of choice for treatment due to its history of rapid symptom resolution and overall fewer treatment failures. Although antibiotic treatment will clear the infection, it will not kill the bacterial spores. In 27% of cases, relapse occurs within 3 weeks of antibiotic termination. In extreme cases, colectomy with end ileostomy may be necessary. Treatment for asymptomatic cases is not recommended.
An innovative CDI treatment may be on the horizon. Researchers have shown that C. difficile infection arises as the result of the disruption of natural flora in the intestines, a condition known as dysbiosis. New research in the treatment of CDI involves isolating specific gut bacteria in the fecal matter of healthy individuals and incorporating it into the gut of a person with CDI to restore normal flora and cure the infection.
CDI can be catastrophic to patients and indeed to entire healthcare facilities if an outbreak occurs. To prevent CDI, follow these guidelines from the CDC:
- Immediately isolate patients with confirmed C. difficile infection and use contact precautions for the duration of diarrhea. Consider extending precautions beyond the duration of diarrhea and using presumptive contact precautions for patients with diarrhea pending confirmed C. difficile diagnosis.
- Educate healthcare personnel, patients, their families, and any visitors about C. difficile and help them maintain contact precautions.
- Follow proper handwashing techniques. Hand hygiene for C. difficile must include vigorous washing of hands with soap and water to mechanically remove spores. Alcohol-based hand rubs are not effective against C. difficile.
- Because C. difficile spores can survive on objects for long periods of time be sure to thoroughly clean and disinfect equipment and objects in the environment. Consider use of sodium hypochlorite (bleach)–containing agents or EPA-registered disinfectants with sporicidal claim for environmental cleaning.
- Enact a laboratory-based alert system for immediate notification of positive test results.
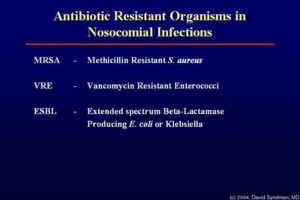
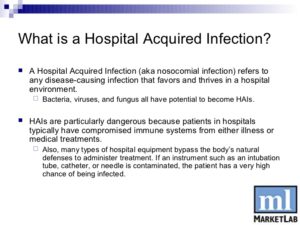
2- MRSA Methicillin-resistant Staphylococcus aureus (MRSA), also known as multidrug resistant S. aureus, includes any strain of S. aureus that has become resistant to the group of antibiotics known as beta-lactam antibiotics. Included in this group are the penicillins (methicillin, amoxicillin, oxacillin) and cephalosporins. Staphylococcus aureus includes gram-positive, nonmotile, non-spore-forming cocci that can be found alone, in pairs, or in grapelike clusters.
When penicillin was first introduced in the early 1940s, it was considered to be a wonder drug because it reduced the death rate from Staphylococcus infection from 70% to 25%. Unfortunately, by 1944, drug resistance was beginning to occur, so methicillin was synthesized, and, in 1959, it became the world’s first semisynthetic penicillin. Shortly thereafter in 1961, staphylococcal resistance to methicillin began as well, and the name “methicillin-resistant S. aureus” and the acronym MRSA were coined. Although methicillin was discontinued in 1993, the name and acronym have remained because of MRSA history.
MRSA is now the most common drug-resistant infection acquired in healthcare facilities. In addition to becoming more problematic as a top HAI in recent years, transmission of MRSA has also become more common in children, prison inmates, and sports participants. Community-associated MRSA (CA-MRSA) most often presents in the form of skin infections. Hospital-acquired MRSA (HA-MRSA) infections manifest in various forms, including bloodstream infections, surgical site infections, and pneumonia. Although approximately 25–30% of persons are colonized in the nasal passages with Staphylococcus, less than 2% are colonized with MRSA. MRSA are extremely resistant and can survive for weeks on environmental surfaces. Transfer of the pathogen can occur directly from patient contact with a contaminated surface or indirectly as healthcare workers touch contaminated surfaces with gloves or hands and then touch a patient.
Risk factors for healthcare-acquired MRSA infection include advanced age, young age, use of quinolone antibiotics, and extended stay in a healthcare facility. Those with diabetes, cancer, or a compromised immune system are also at increased risk of infection.
Symptoms of MRSA infection vary depending on the type and stage of infection and the susceptibility of the organism. Skin infections may appear as painful, red, swollen pustules or boils; as cellulitis; or as a spider bite or bump. They can be found in areas where visible skin trauma has occurred or in areas covered by hair. Patients may also have fever, headaches, hypotension, and joint pain. Complications of MRSA-related skin infections include endocarditis, necrotizing fasciitis, osteomyelitis, and sepsis.
Patient history of admission to a healthcare facility is useful in diagnosing HA-MRSA. Definitive diagnosis of MRSA is made by oxacillin/methicillin resistance that is shown by lab culture and susceptibility testing. Specimens submitted for testing vary depending on the site of suspected infection and may include tissue, wound drainage, sputum, respiratory secretions, and blood or urine cultures.
Treatment for MRSA infections varies based on site of infection, stage of infection, and age of the individual. Treatment includes drainage of abscesses, surgical debridement, decolonization strategies, and antimicrobial therapy with antibiotics such as vancomycin, clindamycin, daptomycin, linezolid, rifampin, trimethoprim-sulfamethoxazole (TMP-SMX), quinupristin-dalfopristin, telavancin, and tetracyclines (limited use). MRSA is rapidly becoming resistant to rifampin; therefore, this drug should not be used alone in the treatment of MRSA infections. Consultation with an infectious disease specialist is recommended for treatment of severe MRSA infections.
3-VRE- Vancomycin-Resistant Enterococci Infection (VRE) or Enterococci (formerly known as Group D streptococci). VRE are non-spore-forming, gram-positive cocci that exist in either pairs or short chains. They are commonly found in the human intestine or the female genital tract. The most common organism associated with vancomycin-ressistant enterococci (VRE) infection in hospitals is Enterococcus faecium. Enterococcus faecalis is also a cause of human disease. VRE infections can occur in the urinary tract, in wounds associated with catheters, in the bloodstream, and in surgical sites. Enterococci are a common cause of endocarditis, intra-abdominal infections, and pelvic infections.
VRE was first reported in Europe in 1986, followed in 1989 by the first report in the United States. Since then it has spread rapidly. Between 1990 and 1997, the prevalence of VRE in hospital patients increased from less than 1% to 15%.
VRE, which is found predominantly in hospitalized or recently hospitalized patients, are difficult to eliminate because they are able to withstand extreme temperatures, can survive for long periods on environmental surfaces, and are resistant to vancomycin. Transmission of VRE occurs most commonly in the form of person-to-person contact by the hands of healthcare workers after contact with the blood, urine, or feces an infected individual. VRE is also spread from contact with environmental surfaces, or through contact with the open wound of an infected person.
People most at risk for infection with VRE include the elderly and those with diabetes, those with compromised immune systems, and those who are already colonized with the bacteria. Prolonged hospitalization, catheterization (urinary and intravenous), and long-term use of vancomycin or other antibiotics also increase a person’s risk of infection.
Symptoms of VRE infection vary depending on the site of infection and may include erythema, warmth, edema, fever, abdominal pain, pelvic pain, and organ pain. Definitive diagnosis is made by culture and susceptibility testing with specimens obtained from suspected sites of infection