Your risk for meningococcal meningitis increases if you are exposed to the bacterium that causes it. Your risk also increases if you’ve had a recent upper respiratory infection. Babies, children, teens, and the elderly are at greatest risk.
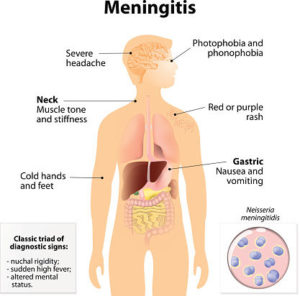
Signs & symptoms of meningococcal meningitis may vary from case to case. The more common S/S:
- General poor feeling
- Sudden high fever
- Severe, persistent headache
- Neck stiffness
- Nausea or vomiting
- Discomfort in bright lights
- Drowsiness or difficulty awakening
- Joint pain
- Confusion or other mental changes
A reddish or purple skin rash (known as petechiae)!!!!! This is a very important sign to watch for. If it does not turn white when you press on it with a glove the rash may be a sign of bacteremia, or a bacterial infection in the bloodstream. This is a medical emergency.
- Tense or bulging soft spot (in babies)
- High-pitched or moaning cry (in babies)
- Stiff, jerky movements or floppiness (in babies or toddlers)
- Irritability
- Fast breathing
- Lethargy or excessive sleepiness
- Blotchy skin, turning pale or blue
- Shivering, or cold hands and feet
- Seizure
Meningococcal meningitis can cause death or serious complications, such as brain damage, paralysis, gangrene, or deafness. To prevent these problems, it’s important to act quickly. Do not wait. Seek immediate medical attention. Go to an emergency room or call 911 if:
- You notice symptoms of meningococcal meningitis.
- Symptoms do not improve with treatment.
- You think you have been exposed to meningococcal meningitis.
How its diagnosed:
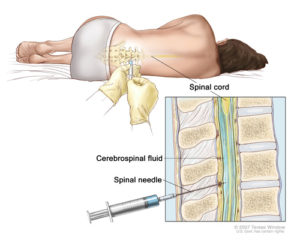
Tests can confirm a diagnosis of meningococcal meningitis; Meningococcal disease can be difficult to diagnose because the signs and symptoms are often similar to those of other illnesses. If a doctor suspects meningococcal disease, they will collect samples of blood or cerebrospinal fluid (fluid near the spinal cord). Doctors then send the samples to a laboratory for testing.
Treatments:
The doctor may start antibiotics, such as penicillin or ceftriaxone, by an IV, or intravenous line. You or your child may also need other medication to treat problems related to increased spinal fluid pressure. Doctors sometimes prescribe steroids for antiinflammatory effect or the spinal cord. Penicillin is the drug of choice for the treatment of meningococcal meningitis and septicemia. Chemoprophylactic antimicrobials most commonly used to eradicate meningococci include rifampin, quinolones (eg, ciprofloxacin), ceftriaxone. Also included in this class are minocycline and spiramycin.
Meningococcal meningitis is a serious disease — even with treatment. That’s why prevention is a far better approach. The meningococcal vaccine can prevent meningitis infection. In the U.S., three types of meningococcal vaccines are used that are:
- Meningococcal conjugate vaccine (MCV4) — is approved for people ages 9 months to 55.
- Meningococcal polysaccharide vaccine (MPSV4) — This vaccine was approved in the 1970s and protects against most forms of meningococcal disease. This vaccine used is for people as young as 9 months and older than age 55.
- Serogroup B Meningococcal B (MenB) – Both are licensed for ages 10-24 but can be used in older patients also.