Causes of muscle atrophy
Unused muscles can waste away if you are not active. Even after it begins, this type of atrophy can often be reversed with exercise and improved nutrition.
Muscle atrophy can also happen if you are bedridden or unable to move certain body parts due to a medical condition. Astronauts, for example, can also experience some muscle atrophy after a few days of weightlessness.
Other causes for muscle atrophy include:
- lack of physical activity for an extended period of time
- aging
- alcohol-associated myopathy, a pain and weakness in muscles due to excessive drinking over long periods of time
- burns
- injuries, such as a torn rotator cuff or broken bones
- malnutrition
- spinal cord or peripheral nerve injuries
- stroke
- long-term corticosteroid therapy
Diseases can cause muscles to waste away or can make movement difficult, leading to muscle atrophy. These include:
- amyotrophic lateral sclerosis (ALS), also known as Lou Gehrig’s disease, affects nerve cells that control voluntary muscle movement
- dermatomyositis, causes muscle weakness and skin rash
- Guillain-Barré syndrome, an autoimmune disease that leads to nerve inflammation and muscle weakness
- multiple sclerosis, an autoimmune disease in which the body destroys the protective coverings of nerves
- muscular dystrophy, an inherited disease that causes muscle weakness
- neuropathy, damage to a nerve or nerve group, resulting in loss of sensation or function
- osteoarthritis, causes reduced motion in the joints
- polio, a viral disease affecting muscle tissue that can lead to paralysis
- polymyositis, an inflammatory disease
- rheumatoid arthritis, a chronic inflammatory disease that affects the joints
- spinal muscular atrophy, a hereditary disease causing arm and leg muscles to waste away
Causes of Spinal Muscular Atrophy:
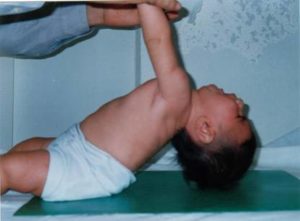
It is caused by a loss of specialized nerve cells, called motor neurons that control muscle movement. In this disease we have an insufficient amount of SMN protein, which leads to permanent loss of motor neurons (Destruction). The weakness tends to be more severe in the muscles that are close to the center of the body (proximal) compared to muscles away from the body’s center (distal). The muscle weakness usually worsens with age.
SMA is an auto-somal recessive disease. This means that (most of the time) both parents must carry the genetic mutation for a child to have the condition.
The gene affected in SMA is the “survival of motor neuron” gene (SMN1 and SMN2). In 95 percent of SMA cases, both copies of the SMN1 gene are missing. All people with SMA have a number of copies of the SMN2 gene. But the SMN2 gene produces only a small amount of functional SMN protein; the more copies of the SMN2 gene a child has, the milder the disease.
If someone in your family has SMA, your chance of being an SMA carrier significantly increases. When both parents are carriers, there is a 1 in 4 (25 percent) chance with each pregnancy that they will have a child with SMA.
The SMA foundation states that the disease generally manifests early in life and is the leading genetic cause of death in infants and toddlers. … One in 40 to one in 50 people (approximately 6 million Americans) are carriers of the SMA gene.
Spinal muscular atrophy (SMA) affects 1 per 8,000 to 10,000 people worldwide. Spinal muscular atrophy type I is the most common type, accounting for about half of all cases. Types II and III are the next most common and types 0 and IV are rare.
Mutations in the SMN1 gene cause all types of spinal muscular atrophy described above. The number of copies of the SMN2 gene modifies the severity of the condition and helps determine which type develops.
The SMN1 and SMN2 genes both provide instructions for making a protein called the survival motor neuron (SMN) protein. Normally, most functional SMN protein is produced from the SMN1 gene, with a small amount produced from the SMN2 gene. Several different versions of the SMN protein are produced from the SMN2 gene, but only one version is functional; the other versions are smaller and quickly broken down. The SMN protein is one of a group of proteins called the SMN complex, which is important for the maintenance of motor neurons. Motor neurons transmit signals from the brain and spinal cord that tell skeletal muscles to tense (contract), which allows the body to move.
Most people with spinal muscular atrophy are missing a piece of the SMN1 gene, which impairs SMN protein production. A shortage of SMN protein leads to motor neuron death, and as a result, signals are not transmitted between the brain and muscles. Muscles cannot contract without receiving signals from the brain, so many skeletal muscles become weak and waste away, leading to the signs and symptoms of spinal muscular atrophy.
Typically, people have two copies of the SMN1 gene and one to two copies of the SMN2 gene in each cell. However, the number of copies of the SMN2 gene varies, with some people having up to eight copies. In people with spinal muscular atrophy, having multiple copies of the SMN2 gene is usually associated with less severe features of the condition that develop later in life. The SMN protein produced by the SMN2 genes can help make up for the protein deficiency caused by SMN1 gene mutations. People with spinal muscular atrophy type 0 usually have one copy of the SMN2 gene in each cell, while those with type I generally have one or two copies, those with type II usually have three copies, those with type III have three or four copies, and those with type IV have four or more copies. Other factors, many unknown, also contribute to the variable severity of spinal muscular atrophy.
Spinal muscular atrophy is inherited in an autosomal recessive pattern, which means both copies of the SMN1 gene in each cell have mutations. In most cases, the parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition. In rare cases, a person with spinal muscular atrophy inherits an SMN1 gene mutation from one parent and acquires a new mutation in the other copy of the gene that occurs during the formation of reproductive cells (eggs or sperm) or in early embryonic development. In these cases, only one parent is a carrier of the SMN1 gene mutation.
Individuals who have more than the usual two copies of the SMN2 gene usually do not inherit the extra copies from a parent. They typically arise during a random error when making new copies of DNA (replication) in an egg or sperm cell or just after fertilization.
Remember SMA is an autosomal recessive disease and this means that (most of the time) both parents must carry the genetic mutation for a child to have the condition.
The gene affected in SMA is the “survival of motor neuron” gene (SMN1 and SMN2). In 95 percent of SMA cases, both copies of the SMN1 gene are missing. All people with SMA have a number of copies of the SMN2 gene. But the SMN2 gene produces only a small amount of functional SMN protein; the more copies of the SMN2 gene a child has, the milder the disease.
If someone in your family has SMA, your chance of being an SMA carrier significantly increases. Remember when both parents are carriers, there is a 1 in 4 (25 percent) chance with each pregnancy that they will have a child with SMA.
Diagnosing:
To find the cause of symptoms, your healthcare provider will perform a physical exam and get a medical history. Your physician may also order one or more of these tests to diagnose SMA:
- Blood test: An enzyme and protein blood test can check for high levels of creatine kinase. Deteriorating muscles release this enzyme into the bloodstream.
- Nerve conduction test: An electromyogram (EMG) measures the electrical activity of nerves muscles and nerves.
- Muscle biopsy: Rarely, a physician may perform a muscle biopsy. This procedure involves removing a small amount of muscle tissue and sending it to a lab for examination. A biopsy can show atrophy, or loss of muscle.
- Genetic test: This blood test identifies problems with the SMN1 gene. As a diagnostic tool, a genetic test is 95% effective at finding the altered SMN1 gene. Some states test for SMA as part of routine newborn screenings.
DNA testing is the preferred testing.
Genetic testing is a type of medical test that identifies changes in chromosomes, genes, or proteins. The results of a genetic test can confirm or rule out a suspected genetic condition or help determine a person’s chance of developing or passing on a genetic disorder. More than 1,000 genetic tests are currently in use, and more are being developed.
Several methods can be used for genetic testing:
- Molecular genetic tests (or gene tests) study single genes or short lengths of DNA to identify variations or mutations that lead to a genetic disorder.
- Chromosomal genetic tests analyze whole chromosomes or long lengths of DNA to see if there are large genetic changes, such as an extra copy of a chromosome, that cause a genetic condition.
- Biochemical genetic tests study the amount or activity level of proteins; abnormalities in either can indicate changes to the DNA that result in a genetic disorder.
Genetic testing is voluntary. Because testing has benefits as well as limitations and risks, the decision about whether to be tested is a personal and complex one. A geneticist or genetic counselor can help by providing information about the pros and cons of the test and discussing the social and emotional aspects of testing.
Newborn Testing: To test if the routine newborn screening dried blood spots can be used to test if missing 2 copies of SMN1 gene, a status indicating spinal muscular atrophy.