Methods of Disease Transmission. There are many insects that are the primary or intermediate hosts or carriers of human diseases. Pathogens that are capable of being transmitted by insects include protozoa, bacteria, viruses, and such helminths as tapeworms, flukes, and roundworms. There are two methods of transmission of a pathogen by insects: mechanical and biological.
The frequency of the diseases mentioned is continuously changing. Some of these have become rare as a result of progress in hygiene and vaccinations measures (yellow fever, Japanese encephalitis, typhus, plague). Others, after having virtually disappeared, are re-emerging (trypanosomiasis). Finally, others are spreading, notably due to possible changes in climate and the changes that this brings about in the ecology of the vectors (dengue fever, chikungunya virus, Lyme disease, etc.). We will briefly present the most common diseases.
Mosquito-borne diseases or mosquito-borne illnesses are diseases caused by bacteria, viruses or parasites transmitted by mosquitoes. They can transmit disease without being affected themselves. Nearly 700 million people get a mosquito-borne illness each year resulting in over one million deaths.
Diseases transmitted by mosquitoes include: malaria, dengue, West Nile virus, chikungunya, yellow fever,] filariasis, tularemia, dirofilariasis, Japanese encephalitis, Saint Louis encephalitis, Western equine encephalitis, Eastern equine encephalitis, Venezuelan equine encephalitis, Ross River fever, Barmah Forest fever, La Crosse encephalitis, and Zika fever, as well as newly detected Keystone virus and Rift Valley fever.
Diseases transmitted onto humans by insects:
Rat Lung Worm.
Angiostrongyliasis, also known as rat lungworm, is a disease that affects the brain and spinal cord. It is caused by a parasitic nematode (roundworm parasite) called Angiostrongylus cantonensis. The adult form of A. cantonensis is only found in rodents, particularly the rat. The rat worm lung life cycle is the adult worm lies it’s eggs in the lung of a rat, the eggs turn into larvae, the larvae are coughed up from the rat’s lungs and swallowed back into it’s stomach. Than they are expelled in the rat’s feces and are eaten by a second host, a slug or a snail. The slug is than eaten by a rat and the process it repeated. The nfected rodents pass larvae of the worm in their feces. Snails, slugs, and certain other animals (including freshwater shrimp, land crabs, and frogs) can become infected by ingesting this larvae; these are considered intermediate hosts. Humans can become infected with A. cantonensis if they eat (intentionally or otherwise) a raw or undercooked infected intermediate host, thereby ingesting the parasite. For more information on the life-cycle of A. cantonensis, visit the CDC website. Areas noted for this disease are Hawaii, these larval worms can be found in raw or undercooked snails or slugs. Sometimes people can become infected by eating raw produce that contains a small infected snail or slug, or part of one. It is not known for certain whether the slime left by infected snails and slugs are able to cause infection. There is no specific treatment for the disease but our medical team has method treatments to get rid of it. However, the Governor’s Joint Task Force on Rat Lungworm Disease recently published preliminary evidence-based clinical guidelines for the diagnosis and treatment of neuroangiostrongyliasis. Their are preventative measures to prevent getting this. The parasites cannot grow or reproduce in humans and will die eventually, causing inflammation. The parasitic lung worm get digested in out GI tract than absorbed in our bloodstream sent to the surface of the brain and they burrough in the brain spreading out into our nervous system. This causes a terribly inflammatory response in the brain and the auto immune system is trying to fight this infection causing more inflammation to the body. 2 ways the rat lung worm is damaging the body; 1-First the worms are borrowing through the body first that causes bleeding, hemmoraging and tissue damage 2=The auto immune response causing swelling can be damaging to the organs like the brain since its increasing pressure more putting it at risk to be deadly (increased pressure in the brain). This increase pressure in the lining of the skull that can go into meningitis being deadly.
Plague
Fleas are the vector for the plague (or black death), which infects man as well as rats and other rodents. There are three forms of plague that occur in humans: bubonic, pneumonic, and septicemic. The bubonic type, in the form of the bacterium, Yersina pestis, is transmitted by fleas. The disease is passed as fleas regurgitate plague bacilli when biting, when flea feces are scratched into the skin, or when the host ingests an infected flea. The plague has killed millions of people in history, especially in the 14th and 17th centuries. In 14th century Europe, the great pandemic resulted in twenty-five million deaths. The plague is still a problem to society, with some 5,000 cases annually.
Enteric diseases.
There are many bacterial diseases that are transmitted by some form of fecal contamination of food or water, either directly or indirectly. House flies are a primary agent in transmitting these diseases, and do so mechanically. Typhoid Fever (Salmonella typhi) is a well-known enteric disease, and affects humans worldwide. Cholera is another enteric disease of great importance. Shigella, causing dysentery and diarrhea, and Escherichia coli, causing urogenital and intestinal infections, are widespread enteric diseases.
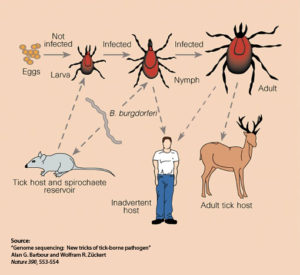
Lyme disease.
This disease is caused by an arachnid, the deer tick, which carries a bacterium called Borrelia bugdorferi. When a person or warm-blooded mammal is bitten, the bacterium enters the bloodstream, and Lyme disease may occur. The disease was first described in New England and the mid-Atlantic states, but is now known from all of the Northern Hemisphere. Mosquitoes can carry the disease also and transmit it via bites.
Sleeping Sickness.
This disease is also known as African Trypanosomiasis. The disease is transmitted by the Tsetse Fly, in the genus Glossina. The causative agent of African trypanosomiasis is Trypanosoma brucei (two forms). The disease is known to have a high mortality rate, not only among people, but among cattle, which was one of the reasons that parts of Africa could not be settled. Wholesale destruction of habitat and reservoir hosts has had some positive impact on the distribution of the disease.
American Trypanosomiasis.
This disease is also known as Chagas’ Disease. Trvpanosoma cruzi, a protozoan and causative agent of Chagas’ Disease, invades the muscle cells of the digestive tract and heart, and sometimes also the skeletal muscle. There the protozoa multiply. Adult trypanosomes may circulate in the blood, but they do not invade blood cells the way malaria parasites do. Transmission of the protozoa is by Conenose Bugs, also known as Kissing Bugs, and is by the bug’s feces, not the bite. Conenose Bugs feed at night on their sleeping victims.
Malaria
Malaria represents the primary health risk for travellers due to being very widespread in the tropical and subtropical regions around the globe and due to its potentially fatal outcome. The disease is caused by a unicellular blood-dwelling parasite of the genus Plasmodium, transmitted by a mosquito of the genus Anopheles. Different species exist. The study of this disease is the subject of a specific sheet.
The chikungunya virus
This is an emerging viral disease caused by an Alphavirus, the main reservoir of which consists of monkeys and other vertebrates including infected humans. The transmission to humans occurs as a result of the bite of the Aedes genus mosquito. This is essentially a diurnal vector. This disease affects Africa, Southeast Asia and the entire Indian subcontinent. The disease progresses in the form of epidemic outbreaks.
The disease can go unnoticed. In its usual form, it leads to a feverish state with intense joint and muscular pains. It is sometimes accompanied by mild haemorrhaging. The disease progression is normally favourable but complications and death can occur. There is a long recovery period with long-lasting residual asthenia. The signs are not very specific, in such a way that without a serology test, the diagnosis can be confused with other diseases causing fever and pain, such as dengue fever, malaria, etc.
No specific anti-viral treatment exists. The treatment is purely symptomatic (paracetamol-type non-salicylate analgesics). The disease confers long-lasting immunity. There is no vaccine; prevention consists of avoiding mosquito bites.
Dengue fever
Dengue Fever is a viral disease caused by a Flavivirus. It is undergoing a strong resurgence. It is transmitted by the bite of a mosquito of the genus Aedes, which reproduces in stagnant water locations around habitations. The disease occurs in Southeast Asia, Australia, Oceania, the Indian Ocean, the Caribbean, America (from Southeastern USA to northern Argentina), and in sub-Saharan Africa. It is endemic in all the overseas French regional départements and territories. It follows an endemic-epidemic transmission pattern. There are 4 distinct serotypes of the disease.
After an incubation period of 7 days, the clinical picture is one of a fever and aches with a rash. After a remission with a drop in temperature, the established stage occurs with resumption of the symptomatology. The disease lasts for a week, the recovery period is long, and is marked by a long-lasting asthenia. There are subclinical forms and, on the contrary, severe forms resulting in death. The clinical picture is not very specific; it is shared by other arboviral infections that present Dengue fever-like syndromes. The definitive diagnosis of isolated cases depends on serology testing.
The treatment is purely symptomatic (paracetamol-type non-salicylate analgesics). A vaccine is under study. The disease resulting from a virus of a given group does not confer immunity with regard to the viruses of the other groups. On the contrary, the fact that a patient has already suffered dengue fever exposes them to a new, more severe illness in the event of a new infection by a virus from a different group.
Yellow fever
Yellow fever is a viral haemorrhagic fever caused by a Flavivirus: the yellow fever virus. It is transmitted by the bite of a mosquito of the Aedes genus. The natural host of the virus is a particular species of monkey living in forest regions. The virus can be transmitted, accidentally, to human communities. The disease follows an endemic-sporadic transmission pattern and gives rise to epidemics. It affects the tropical and subtropical regions of South America and Africa. The disease is absent from Asia, the Pacific and the Indian Ocean. It is currently highly present in Africa where small epidemics are regularly observed (Ivory Coast, Cameroon, Senegal).
The disease typically begins with a highly feverish state with headaches and lower back pain. It then progresses, in the typical forms, in 2 stages. A red stage with fever, congested appearance to the face, headaches. There is a remission in the 3rd-4th day, then a yellow stage with recurrence of the fever, deterioration of the general condition, jaundice, black vomit (vomitus containing blood), haemorrhaging, reduction in urine volume. The progression can be fatal. There are many milder or subclinical forms.
The treatment is purely symptomatic. There is a vaccination that is very effective. This vaccination is compulsory for travellers visiting countries where the disease is likely to exist. The vaccination is administered at the approved vaccination centres. It is subject to inclusion on the international vaccination record.
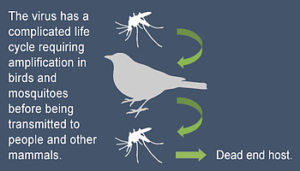
West Nile disease
It is an infection caused by a Flavivirus: the West Nile virus. The vector is a mosquito of the Culex genus. The reservoir of the virus consists of birds. The disease initially affected Africa, part of central and southern Europe, the Middle East, and India. A gradual expansion is being observed with a spread across the American continent from East to West, and to Eastern Europe and Russia. In France, the disease is present in Camargue where it affects horses, but also humans.
The disease is frequently asymptomatic but it can cause feverish states accompanied sometimes by neurological signs presenting a clinical picture of encephalitis or flaccid paralysis. There is a risk of death or serious sequelae.
The treatment is symptomatic. Vaccine trials are underway.
Japanese encephalitis
Japanese encephalitis (JE) is caused by a Flavivirus. It is transmitted to humans via the bite of a mosquito of the Culex genus. The reservoir of the virus consists of wild aquatic animals and pigs, from which the disease can spread to humans in rural areas. JE affects the far south-east of Russia, the whole of Asia, India and the far north of Australia. It is endemic in rural areas with rice fields and irrigation throughout the year. It is epidemic in rural and urban areas during the monsoon. There are 30,000 to 50,000 new cases per year, mainly among children, with 25,000 deaths. The risk of travellers contracting the disease is roughly 1/1,000,000.
There is one visible form (one case) for every 250 contaminations. The clinical picture formed by the visible forms is not specific. It can consist of an isolated feverish state, or a meningitis or meningoencephalitis clinical picture. It is estimated that the mortality rate is 30% and that 30% of patients will recover with sequelae.
The treatment is symptomatic. There is a preventive vaccination. There are two types of vaccines on the market: a cell culture vaccine in Western countries and a suckling mouse brain vaccine. This vaccination is only available at approved vaccination centres.
Vaccination is recommended for :
- Adults who are expatriates or who need to reside for more than 30 days in Asia;
- Adults who are visiting these regions, undertaking significant outdoor activity, in particular in rice fields or marsh areas, during the virus transmission period, in particular during the rainy season, regardless of the duration of the stay. The following activities are considered to present a risk: sleeping outdoors without a mosquito net, camping, working outdoors, cycling, hiking, etc.; especially in areas where flood irrigation is practised.The vaccine marketed in France is currently reserved for persons aged 18 and over.
Filariasis
Filariasis is a group of tropical diseases linked by the development, within the body, of adult worms (filariae) and their lavae or microfilariae. These diseases constitute a real public health problem for the local populations, but infection is rare among travellers. They are transmitted by specific insects acting as vectors, which explains their presence in certain specific areas. A distinction can be made between lymphatic filariasis and cutaneous filariasis depending on whether the adult worms live in the lymphatic system or beneath the skin.
Lymphatic filariasis :
- There are three species: Wuchereria bancrofti (cosmopolitan), Brugia malayi and Brugia timori (Southeast Asia). Each species is transmitted by a specific mosquito (Culex, Anopheles, Aedes, Mansonia) and has a well-defined geographical distribution. The disease is endemic in tropical regions where 120 million people are infected.
- The symptoms are linked with the disruption of the lymphatic drainage caused by the adult worms, giving rise to oedema of the limbs, lymphangitis and superinfections. They are also allergenic in nature due to the microfilariae. Without treatment, the oedema progress to a chronic state, causing a thickening of the tissues and resulting in a clinical presentation of elephantiasis.
- Treatment uses anti-parasitic drugs. The WHO launched a mass treatment program in 2000 aiming to stop the transmission of the disease.
Loa loa filariasis :
- This is a cutaneous filariasis found in the forest regions of central Africa. It is caused by the Loa-loa. It is transmitted by the bite of a horse fly: the Chrysops. The microfilariae live in the blood circulation.
- The symptomatology is characterised by itching, urticarial episodes, migrating oedema of the limbs. The movement of the adult worm beneath the skin is the cause of the tortuous cords; they move at a speed of roughly 1 cm per minute. The passage of the worm beneath the conjunctiva of the eye causes tearing, red eye and foreign body sensation. This occurrence is dramatic but relatively benign. The disease progresses over a long period of time. Later stage complications can be observed, particularly affecting the heart.
- Treatment uses anti-parasitic drugs. They must be used carefully.
Other types of filariasis :
There are other types of filariasis transmitted by specific vectors: Onchocerciasis, filarial pleural effusion. They are rarer.
Sleeping sickness
Human African typanosomiasis or sleeping sickness is a parasite disease caused by the Trypanosoma protozoa (unicellular blood-dwelling parasites), several different species of which exist. This disease, which virtually disappeared during the 1960s as a result of the actions of the major disease mobile teams founded by Jamot, is in full resurgence due to troubles disrupting the various health systems. It is transmitted by the bite of a fly: Glossina or tsetse fly. It is found only in Africa. It is found in homes in the tropical and subtropical regions. The disease affects rural populations; the risk to travellers is limited.
The disease progresses in two stages: a lymphatic/blood stage during which the parasite is found in the lymphatic system, then a stage called the “neurological phase” where the central nervous system is affected. The progression occurs over a long period of time. Without treatment, the disease is invariably fatal.
The disease is treated with anti-parasite drugs; the treatment is very well codified but relatively hard to undergo. It is very effective.
The leishmaniases
The leishmaniases are parasite diseases caused by Leishmania (unicellular parasites that infect the reticulohistiocytic system) transmitted by a species of sand fly (subfamily Phlebotominae). A distinction can be made, according to the type of parasite, between the cutaneous, mucocutaneous and visceral forms.
The cutaneous and mucocutaneous forms have a different aspects on the American continent compared with Asia. The various forms of the disease have as a common feature, the creation of chronic ulcers, more or less hollow, without a tendency to heal.
The visceral forms or Kala-azar are observed in the Mediterranean basin. They are characterised by a severe deterioration of the general condition of the patient with an increase in the size of the lymph nodes and of the spleen, and a drop in blood cell numbers.
These diseases have specific treatments, which need to be followed over long periods of time in order to achieve a cure.
Lyme disease
Lyme disease is an infection caused by a a species of bacteria of the Borrelia genus: Borrelia burgdorferi transmitted by the bite of a tick of the Ixodes genus. 10 to 15% of them carry the Borrelia bacteria. The risk of contamination by tick bite varies between 1 and 6% depending on the region. The disease is found in the northern hemisphere, in America and in Eurasia during the active phase of the ticks, between May and October. It is not uncommon in France.
The disease begins with a red skin lesion centred around the tick bite that gradually spreads out and ends up disappearing within a few days or a few weeks. A few weeks or a few months later, other signs may appear, involving the joints, the nervous system (paralysis and pain), heart rhythm abnormalities and, more rarely, other symptoms. The expression of the disease is usually more severe in Northern America than in Europe.
The treatment relies on antibiotics. Admission to hospital can be necessary.
Tick-borne meningoencephalitis
Tick-borne meningoencephalitis is a disease of the central nervous system caused by a Flavivirus (Tick Born Encephalitis Virus). It is transmitted by the bite of a tick of genus Ixode, in spring and summer. In the past, a distinction was made between the European forms (Central Europe and Eastern Europe) and the Asian forms (from Russia to Japan), but in fact it consists of the same disease transmitted by different tick species. In the areas affected, the disease is restricted to limited territories. It has been expanding continuously over the last few years. The disease is present in Alsace.
After an incubation period of 7 days, the symptomatology progresses in two stages. A first stage that lasts 2 to 4 days is characterised by a flu-like state. The second stage does not always occur, and if it does, appears 10 days later. It is characterised by neurological signs of varying severity: meningitis, meningoencephalitis, meningo-encephalo-radiculitis. In general the disease progresses towards recovery. Sequelae can be observed. The mortality rate is 1%.
The treatment is purely symptomatic; there is no medicine that acts on the virus itself. A preventive vaccine is available. The vaccination against tick-borne encephalitis is recommended for travellers staying in endemic rural and forest regions in central, eastern and northern Europe, between spring and autumn.
The tick-borne spotted fevers
The tick-borne spotted fevers are diseases caused by bacteria of the Rickettsia genus. They are transmitted by tick bites. More than 20 species of the Rickettsia genus are pathogenic for humans. Besides the various spotted fevers, they are responsible for typhus (epidemic typhus, endemic typhus, scrub typhus).
The spotted fevers are found in Europe, on the North American continent and in sub-Saharan Africa (especially southern). Various types of the disease have been described: Mediterranean spotted fever, Israeli tick typhus, Indian tick typhus, Rocky Mountain spotted fever, African tick bite fever.
These various diseases present a common symptomatology. After an incubation period of 5 days, the following signs appear: fever, an eschar at the point of the tick bite with satellite lymphadenopathy (lymph glands) and, not systematically, skin rash with blisters. Progression can be severe for Mediterranean spotted fever and especially Rocky Mountain spotted fever. For the other types of the disease, progression is benign.
The severe forms are treated with antibiotics.