Genetic and environmental influences
While there currently is no identified genetic locus/loci associated with Alice in Wonderland Syndrome, observations suggest that a genetic component does exist. AiWS does appear to be passed on from parent to child, with one case study showcasing a grandmother, mother, son, and daughter all with Alice in Wonderland Syndrome. In addition, there is an established hereditary trait of migraines. Examples of environmental influences on the incidence of AiWS include the use of the drug topiramate and potentially the dietary intake of tyramine. Further research is required to establish the genetic and environmental influences on Alice in Wonderland Syndrome.
Alice in Wonderland
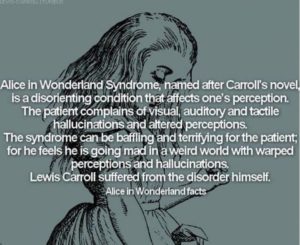
Alice in Wonderland Syndrome was named after Lewis Carroll’s famous 19th-century novel Alice’s Adventures in Wonderland. In the story, Alice, the title character, experiences numerous situations similar to those of micropsia and macropsia. The thorough descriptions of metamorphosis clearly described in the novel were the first of their kind to depict the bodily distortions associated with the condition. Speculation has arisen that Carroll may have written the story using his own direct experience with episodes of micropsia resulting from the numerous migraines he was known to suffer from. It has also been suggested that Carroll may have suffered from temporal lobe epilepsy.
Gulliver’s Travels
Alice in Wonderland Syndrome’s symptom of micropsia has also been related to Jonathan Swift’s novel Gulliver’s Travels. It has been referred to as “Lilliput sight” and “Lilliputian hallucination”, a term coined by British physician Raoul Leroy in 1909, based on the small people that inhabited the island of Lilliput in the novel.
Etiology
Complete and partial forms of the Alice in Wonderland syndrome exist in a range of disorders, including epilepsy, intoxicants, infectious states, fevers, and brain lesions. Furthermore, the syndrome is commonly associated with migraines, as well as the use of psychoactive drugs. It can also be the initial symptom of the Epstein–Barr virus (see mononucleosis), and a relationship between the syndrome and mononucleosis has been suggested. Epstein-Barr Virus appears to be the most common cause in children, while for adults it is more commonly associated with migraines.
Cerebral hypotheses
AiWS can be caused by abnormal amounts of electrical activity causing abnormal blood flow in the parts of the brain that process visual perception and texture. Nuclear medical techniques using technetium, performed on patients during episodes of Alice in Wonderland syndrome, have demonstrated that AiWS is associated with reduced cerebral perfusion in various cortical regions (frontal, parietal, temporal and occipital), both in combination and in isolation. It has been hypothesized that any condition resulting in a decrease in perfusion of the visual pathways or visual control centers of the brain may be responsible for the syndrome. For example, one study used single photon emission computed tomography to demonstrate reduced cerebral perfusion in the temporal lobe in patients with AiWS. Other theories exist that suggest the syndrome is a result of unspecific cortical dysfunction (e.g. from encephalitis, epilepsy, decreased cerebral perfusion), or reduced blood flow to other areas of the brain. Other theories suggest that disordered body image perceptions stem from within the parietal lobe. This has been demonstrated by the production of disturbances of body image through electrical stimulation of the posterior parietal cortex. Other researchers suggest that metamorphopsias may be a result of reduced perfusion of the non-dominant posterior parietal lobe during migraine episodes.
Throughout all the neuroimaging studies, several cortical regions (including the temporoparietal junction within the parietal lobe, and the visual pathway, specifically the occipital lobe) are associated with the development of Alice in Wonderland syndrome symptoms.
Migraines
The role of migraines in Alice in Wonderland syndrome is still not understood, but both vascular and electrical theories have been suggested. For example, visual distortions may be a result of transient, localized ischaemia (an inadequate blood supply to an organ or part of the body) in areas of the visual pathway during migraine attacks. In addition, a spreading wave of depolarization of cells (particularly glial cells) in the cerebral cortex during migraine attacks can eventually activate the trigeminal nerve’s regulation of the vascular system. The intense cranial pain during migraines is due to the connection of the trigeminal nerve with the thalamus and thalamic projections onto the sensory cortex. Alice in Wonderland syndrome symptoms can precede, accompany, or replace the typical migraine symptoms.
Diagnosis
Alice in Wonderland syndrome is a disturbance of perception rather than a specific physiological change to the body’s systems. The diagnosis can be presumed when other causes have been ruled out and if the patient presents symptoms along with migraines and complains of onset during the day (although it can also occur at night). As there are no established diagnostic criteria for Alice in Wonderland syndrome, there is likely to be a large degree of variability in the diagnostic process and thus it is likely to be poorly diagnosed.
Prognosis
Whatever the cause, the bodily related distortions can recur several times a day and may take some time to abate. Understandably, the person can become alarmed, frightened, and panic-stricken throughout the course of the hallucinations—maybe even hurt themselves or others around them. The symptoms of the syndrome themselves are not harmful and are likely to disappear with time. The outcome is typically not harmful, especially in children, and most patients outgrow these episodes. The long-term prognosis typically depends on the root cause of the syndrome, and it is the underlying condition which must be evaluated and treated. Often, the difficulty lies within the patient’s reluctance to describe their symptoms out of fear of being labeled with a psychiatric disorder.
Treatment
At present, Alice in Wonderland syndrome has no standardized treatment plan. Often, treatment methods revolve around migraine prophylaxis, as well as the promotion of a low tyramine diet. Drugs that may be used to prevent migraines include: anticonvulsants, antidepressants, calcium channel blockers, and beta blockers. Other treatments that have been explored include repetitive transcranial magnetic stimulation (rTMS). Further research is required to establish an effective treatment regime.
Epidemiology
The lack of established diagnostic criteria or large-scale epidemiological studies on Alice in Wonderland syndrome means that the exact prevalence of the syndrome is currently unknown. One study on 3,224 adolescents in Japan demonstrated the occurrence of macropsia and micropsia to be 6.5% in boys and 7.3% in girls, suggesting that the symptoms of AiWS may not be so rare.
It appears that the male/female ratio is dependent on the age range being observed. Studies showed that younger males (age range of 5 to 14 years) were 2.69 times more likely to experience AiWS than girls of the same age, while there were no significant differences between students of 13 to 15 years of age. Conversely, female students (16- to 18-year-olds) showed a significantly greater prevalence.
The average age of the start of Alice in Wonderland syndrome is six but it is very normal for some to experience the syndrome from childhood to their late 20’s. It is also thought that this syndrome is hereditary because many parents who have AiWS report their children having it as well.