 C
C
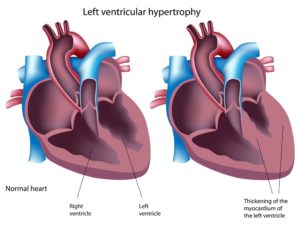
 Heart Enlarged
Heart Enlarged
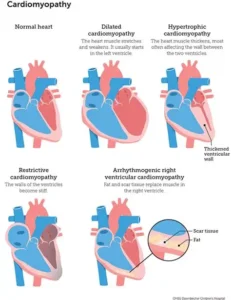
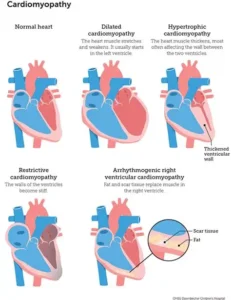
Cardiomyopathy is cardiomyopathy, meaning rather in adult or child the same problems in each age group occur but degree of the disease varies for all, it is case by case. What is cardiomyopathy?
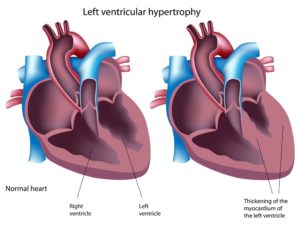
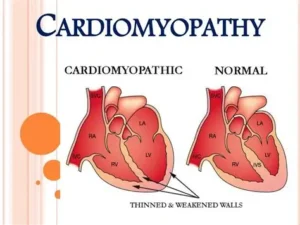
Cardiomyopathy is a disease of the heart muscle characterized by an abnormally large, thick or stiff heart muscle. It may affect only the heart’s lower chambers (ventricles) or both the lower and upper chambers (atria). For an adult there just more wear and tear on the organ due to age and severity of the disease.
Cardiomyopathy causes damage to tissue around the heart, as well as heart muscle cells. In severe cases, the heart becomes so weak that it can’t pump blood properly. This can lead to heart failure or irregular heartbeats (arrhythmias). In some cases, cardiomyopathy also involves a buildup of scar tissue or fat within the heart muscle. In rare cases, the heart muscle can’t relax and blood can’t fill the heart properly.
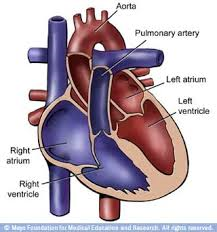
Remember the natural pacemaker in humans is located in the upper right chamber (Rt. atrium) in the upper right region called the sinus node. The sinus node initiates our impulses from that right atrium across to the Lt. atrium and works the impulse sensation down thru the A-V node-atrioventricular node (site between upper and lower chambers in the heart located at the inferior end of the interatrial septum ending at the top of the ventricles in the heart)). From the A-V node the impulse sensation continues on from A-V node to the end of the lower right and left lower chambers (called the ventricles) of the heart that continues up the ventricles and passing through the bundle of His to the bundle branches/Purkinje fibers (The bundle of His is an important part of the electrical conduction system of the heart, as it transmits impulses from the A-V node, located at the inferior end of the interatrial septum, to the ventricles of the heart). Than the impulse sensation goes located in the inner ventricular walls of the heart radiating over the outside of the ventricles = Purkinje Fibers. This whole process allows the heart beat to occur sounding “LubDub”.
This entire impulse conduction process allows the heart to fill up the chambers with blood first in upper chambers to lower ones to releasing the blood in the ventricles (the Rt Ventricle pumps blood to the heart to get more oxygen from lungs that sends this fresh oxygenated blood to the left side of the heart. The left ventricle pumps the filling of its blood into our blood stream called Cardiac Output in creating the heart to beat. Stroke Volume x Heart Rate=our Cardiac Output (SVxHR=CO). Stroke volume is the amount of blood circulated by the heart with each beat x HR = beat in 60 secs.
Cardiomyopathy is very often a “time-will-tell” disease. Symptoms can vary and the progression of the disease can be unpredictable. There are many forms of cardiomyopathy; just like in the adult.
What are the types of cardiomyopathy?
The main types include:
Dilated cardiomyopathy (DCM)
DCM is the most common type and occurs when the main pumping chamber of the heart muscle is too stretched out (dilated). Dilated cardiomyopathy makes the heart unable to pump blood effectively.
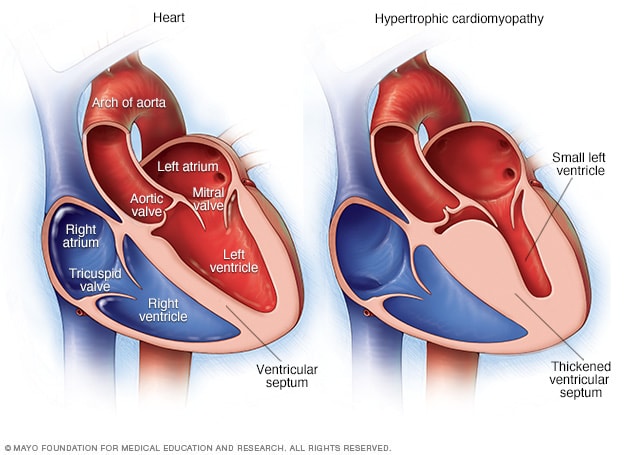
Hypertrophic cardiomyopathy (HCM)
HCM makes the heart muscle too thick. Usually, the thickening occurs in the muscle of the left ventricle in the heart, often involving the wall between the heart’s two ventricles.
Restrictive cardiomyopathy
Restrictive cardiomyopathy is a rare type of cardiomyopathy that causes the heart muscle to become very rigid or stiff. This makes it difficult for the ventricles of the heart to properly fill with blood.
Arrhythmogenic right ventricular cardiomyopathy (ARVC)
ARVC is a rare form of cardiomyopathy that affects only one in 5,000 people. It occurs when the muscle of the heart’s right ventricle is replaced by thick or fatty scar tissue. The scarring “scrambles” electrical signals within the heart and can make it difficult for the heart to pump blood.
Remember the sinus node (natural pacemaker) of the heart.
How Cardiomyopathy is diagnosed:
Because the symptoms of cardiomyopathy can be diverse, it is often misdiagnosed as asthma, an infection or a gastrointestinal problem but the tests similar to adults tests being ruled out for this disease. Remember its the same problem at a different age.
In children who have no symptoms, cardiomyopathy is sometimes diagnosed when the child has a chest x-ray that shows an enlarged heart or an echocardiogram for another reason.
If your child’s doctor suspects cardiomyopathy, he or she may order one or more of the following tests, from least invasive to most invasive tests:
- blood tests
- chest x-rays
- electrocardiogram (EKG or ECG)
- echocardiogram (cardiac ultrasound)
- cardiac magnetic resonance imaging (MRI)
- stress echocardiography, which uses ultrasound and heart-rate monitoring to assess your child’s heart function just before and just after exercise
- stress test, or exercise test
- cardiac catheterization
- coronary angiography
What are the treatment (Rx) options for cardiomyopathy, again similar to adults Rx.?
Your child’s treatment options will be determined by the type of cardiomyopathy he or she has, as well as the specific symptoms. A child with no symptoms might not need medication or other treatment right away. Instead, the cardiologist will monitor your child to gauge the progression of the disease.
A child with more serious symptoms may need additional tests to give the treatment team more detailed information about how the cardiomyopathy is affecting the heart and the rest of the body. .
Many children with cardiomyopathy do well with medication alone. Others need surgery to improve the function of valves, and in the most severe cases, some children need a heart transplant.
Medication for cardiomyopathy
There are several different types of medications for cardiomyopathy, depending on which type your child has and the symptoms.
- Angiotestin converting enzyme (ACE) inhibitors are drugs that dilate blood vessels in the body, fighting the constricting effect caused by heart failure.
- Antiarrhythmic medications combat the abnormal heart rhythms caused by irregular electrical activity within the heart.
- Beta blockers block certain chemicals from binding to nerve receptors in the heart, slowing the heart rate and lowering blood pressure.
- Blood thinners or anticoagulants help prevent the formation of blood clots, especially in children with the dilated form of cardiomyopathy.
- Diuretics prevent the buildup of fluid in the body and can help breathing by reducing fluid in the lungs. These drugs may also be helpful in treating scar tissue on the heart.
Surgical treatments for cardiomyopathy
There are several options for treating cardiomyopathy using surgery or minimally-invasive procedures.
Defibrillators
For some children with cardiomyopathy — particularly HCM — an implantable cardioverter-defibrillator (ICD) can be a life-saving option. This tiny instrument, about the size of a deck of cards, is placed in the chest to monitor the child’s heartbeat. If the child has an arrhythmia, the defibrillator will administer a precise electrical pulse to restore normal heart rhythm.
Pacemakers
Pacemaker implantation is minimally invasive option for some children with cardiomyopathy. The pacemaker — a small electronic device — is inserted directly under the skin, where it sends electric signals to the child’s heart, controlling and monitoring the heart rate. The procedure can be performed under local anesthesia in a matter of hours.
Radiofrequency ablation
Radiofrequency ablation is another type of minimally invasive treatment that can be very effective for some children with cardiomyopathy due to arrhythmia. A small, needle-like probe is inserted into the scarred tissue of the heart muscle, sending out radiofrequency waves that burns away the scar tissue and the arrhythmia.
Surgical removal of some heart muscle
In serious cases of hypertrophic cardiomyopathy, the treatment team may perform a surgery called a septal myectomy or septal myomectomy. This procedure involves the removal of a portion of the thickened muscle in the heart, widening the channel in the heart’s ventricle that leads to the aortic valve. The procedure has a very good success rate, and most children have improved blood flow throughout the heart and body.
Ventricular assist device
In certain types of cardiomyopathy, a ventricular-assist device (VAD) can be used to help recover the heart and normalize the heart’s function. After the heart’s function has returned to normal, the VAD will be removed and the child will be monitored for any further heart problems. This approach using the VAD is called a “bridge to recovery.”
Heart transplant
Children with the most severe cases of cardiomyopathy may need a heart transplant if other methods don’t manage symptoms. While your child is waiting for an available heart, a VAD may be used to support the heart. In many cases, children can return to school and other activities while waiting for a transplant.
So similar to how adults are treated also with cardiomyopathy. The age is the pretty much the difference.

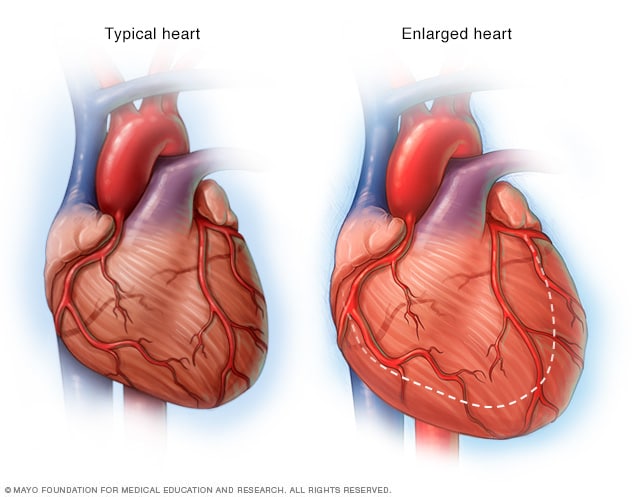
 Heart Enlarged
Heart Enlarged