Children eye health and safety month
August Is Children’s Eye Health and Safety Month!
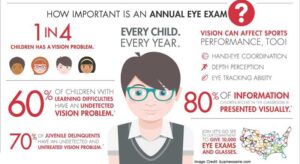
It’s almost back-to-school time and are you prepared with your child’s enrollment forms, orientation schedules, and immunizations–but what about their eyes?
August is Children’s Eye Health and Safety Month—a great signal for you to get your child’s eyes checked before school starts.
Let’s Talk Eye Safety:
Use this month to discuss the importance of eye safety with your children.
CDC states “Approximately 6.8% of children younger than 18 years in the United States have a diagnosed eye and vision condition. Nearly 3 percent of children younger than 18 years are blind or visually impaired, defined as having trouble seeing even when wearing glasses or contact lenses.”.
Children should:
- Wear protective eyewear while participating in sports or recreational activities
- Play with are age-appropriate toys. Avoid toys with sharp or protruding parts
One of the best ways to ensure your child keeps his/her good vision throughout life is to set a good health example.
Talk to your child’s pediatrician if you suspect your child has any of the eye diseases below:
-Amblyopia (lazy eye) – also known as lazy eye, is a vision development disorder in which an eye fails to achieve normal visual acuity, even with prescription eyeglasses or contact lenses. Amblyopia begins during infancy and early childhood. In most cases, only one eye is affected. However, a common cause of amblyopia is strabismus. So if you notice your baby or young child has crossed eyes or some other apparent eye misalignment, schedule an appointment for a children’s eye exam immediately — preferably with an optometrist or ophthalmologist who specializes in children’s vision.
Another clue that your child may have amblyopia is if he or she cries or fusses when you cover one eye.
You can try this simple screening test at home by simply covering and uncovering your child’s eyes (one eye at a time) when he or she is performing a visual task, such as watching television.
-Strabismus (crossed eyes) – Strabismus is a condition that interferes with binocular vision because it prevents a person from directing both eyes simultaneously towards the same fixation point; the eyes do not properly align with each other. Heterotropia is a medical synonym for the condition. Colloquial terms for strabismus include “cross-eye”, “wall-eye”, and a “cast of the eye”. Strabismus in children does not go away on its own and strabismus in adults is treatable, so strabismus treatment is necessary.
-Ptosis (drooping of the eyelid) – Ptosis” is the medical term for a drooping upper eyelid. Eyelid drooping can sometimes affect your vision if it’s severe. Ptosis isn’t a disease. It’s actually a symptom of a condition that you should seek treatment for. Many things can cause ptosis. Some causes being stroke, diabetic neuropathy, myasthenia gravis, muscular dystrophy, botulism, brain aneurysm, adult brain tumor, pituitary cancer, & necrotizing vaculitis. An eye doctor will diagnose ptosis by carefully examining the eyelids. He or she will take detailed measurements of the height of the eyelids and will assess the strength of the eyelid muscles.Surgery can be an effective treatment for ptosis in both children and adult, improving vision as well as cosmetic appearance. It is very important that children with ptosis have regular ophthalmic examinations early in life to monitor their vision and prevent severe vision loss from untreated amblyopia..
-Color deficiency (color blindness) – Two of the most common inherited forms of color blindness are protanopia and deuteranopia. Color vision deficiency (sometimes called color blindness) represents a group of conditions that affect the perception of color. Red-green color vision defects are the most common form of color vision deficiency which is in about 8 percent and 0.5 percent of females of European (northern) ancestry. Affected individuals have trouble distinguishing between some shades of red, yellow, and green. Blue-yellow color vision defects (also called tritan defects), which are rarer, cause problems with differentiating shades of blue and green and cause difficulty distinguishing dark blue from black. These two forms of color vision deficiency disrupt color perception but do not affect the sharpness of vision (visual acuity).
A less common and more severe form of color vision deficiency called blue cone monochromacy causes very poor visual acuity and severely reduced color vision. Affected individuals have additional vision problems, which can include increased sensitivity to light (photophobia), involuntary back-and-forth eye movements (nystagmus), and nearsightedness (myopia). Blue cone monochromacy is sometimes considered to be a form of achromatopsia, a disorder characterized by a partial or total lack of color vision with other vision problems
-Refractive errors (nearsightedness, farsightedness and astigmatism) – The most common types of refractive errors are myopia, hyperopia, presbyopia, and astigmatism. Myopia (nearsightedness) is a condition where objects up close appear clearly, while objects far away appear blurry. With myopia, light comes to focus in front of the retina instead of on the retina.
What are refractive errors?
Refractive errors occur when the shape of the eye prevents light from focusing directly on the retina. The length of the eyeball (longer or shorter), changes in the shape of the cornea, or aging of the lens can cause refractive errors.
What is refraction?
Refraction is the bending of light as it passes through one object to another. Vision occurs when light rays are bent (refracted) as they pass through the cornea and the lens. The light is then focused on the retina. The retina converts the light-rays into messages that are sent through the optic nerve to the brain. The brain interprets these messages into the images we see.
Frequently Asked Questions about Refractive Errors
What are the different types of refractive errors?
The most common types of refractive errors are myopia, hyperopia, presbyopia, and astigmatism.
Myopia (nearsightedness) is a condition where objects up close appear clearly, while objects far away appear blurry. With myopia, light comes to focus in front of the retina instead of on the retina.
Hyperopia (farsightedness) is a common type of refractive error where distant objects may be seen more clearly than objects that are near. However, people experience hyperopia differently. Some people may not notice any problems with their vision, especially when they are young. For people with significant hyperopia, vision can be blurry for objects at any distance, near or far.
Astigmatism is a condition in which the eye does not focus light evenly onto the retina, the light-sensitive tissue at the back of the eye. This can cause images to appear blurry and stretched out.
Presbyopia is an age-related condition in which the ability to focus up close becomes more difficult. As the eye ages, the lens can no longer change shape enough to allow the eye to focus close objects clearly.
Risk Factors
Who is at risk for refractive errors?
Presbyopia affects most adults over age 35. Other refractive errors can affect both children and adults. Individuals that have parents with certain refractive errors may be more likely to get one or more refractive errors.
Symptoms and Detection
What are the signs and symptoms of refractive errors?
Blurred vision is the most common symptom of refractive errors. Other symptoms may include:
- Double vision
- Haziness
- Glare or halos around bright lights
- Squinting
- Headaches
- Eye strain
-
How refractive errors are diagnosed?
- An eye care professional can diagnose refractive errors during a comprehensive dilated eye examination. People with a refractive error often visit their eye care professional with complaints of visual discomfort or blurred vision. However, some people don’t know they aren’t seeing as clearly as they could.
-
How are refractive errors treated?
- Eyeglasses are the simplest and safest way to correct refractive errors. Your eye care professional can prescribe appropriate lenses to correct your refractive error and give you optimal vision.If you have certain eye conditions you may not be able to wear contact lenses. Discuss this with your eye care professional.
- Refractive Surgery aims to change the shape of the cornea permanently. This change in eye shape restores the focusing power of the eye by allowing the light rays to focus precisely on the retina for improved vision. There are many types of refractive surgeries. Your eye care professional can help you decide if surgery is an option for you.
- Contact Lenses work by becoming the first refractive surface for light rays entering the eye, causing a more precise refraction or focus. In many cases, contact lenses provide clearer vision, a wider field of vision, and greater comfort. They are a safe and effective option if fitted and used properly. It is very important to wash your hands and clean your lenses as instructed in order to reduce the risk of infection.
- Refractive errors can be corrected with eyeglasses, contact lenses, or surgery