Know The ear’s role with BPPV
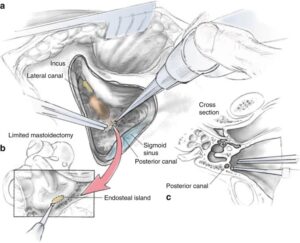
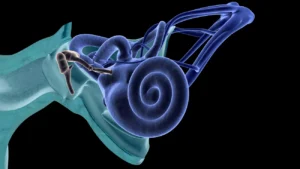
Inside your ear is a tiny organ called the vestibular labyrinth. It includes three loop-shaped structures (semicircular canals) that contain fluid and fine, hair-like sensors that monitor the rotation of your head.
Other structures (otolith organs) in your ear monitor movements of your head — up and down, right and left, back and forth — and your head’s position related to gravity. These otolith organs — the utricle and saccule — contain crystals that make you sensitive to gravity.
For a variety of reasons, these crystals can become dislodged. When they become dislodged, they can move into one of the semicircular canals — especially while you’re lying down. This causes the semicircular canal to become sensitive to head position changes it would normally not respond to. As a result, you feel dizzy. Depending what section of the semicircular canal the problem is in will be a factor with the actual result on the crystals or rocks flowing freely or become stuck together causing a blockage in one of the canals. The other factor that determines this is the etiology for it occuring (ex. Dehydration or blow to the head).
Causes of BPPV;
Timothy C. Hain MD of dizziness and balance.com states The most common cause of BPPV in people under age 50 is head injury . The head injury need not be that direct – -even whiplash injuries have a substantial incidence of BPPV (Dispenza et al, 2011). There is also a strong association with migraine (Ishiyama et al, 2000). BPPV becomes much more common with advancing age (Froeling et al, 1991) and in older people, the most common cause is degeneration of the vestibular system of the inner ear. Viruses affecting the ear such as those causing vestibular neuritis and Meniere’s disease are significant causes(Batatsouras et al, 2012).
Occasionally BPPV follows surgery, including dental work, where the cause is felt to be a combination of a prolonged period of supine positioning, or ear trauma when the surgery is to the inner ear (Atacan et al 2001). While gentamicin toxicity is rarely encountered, BPPV is common in persons who have been treated with ototoxic medications such as gentamicin (Black et al, 2004). In half of all cases, BPPV is called “idiopathic,” which means it occurs for no known reason. Other causes of positional symptoms are discussed here.
Web MD points out tiny calcium “stones” inside your inner ear canals help you keep your balance. Normally when you move a certain way, such as when you stand up or turn your head, these stones move around. But things like infection or inflammation can stop the stones from moving as they should. This unfortunately sends a false message to your brain and causes the vertigo. About half the time, doctors can’t find a specific cause for BPPV.
When a cause can be determined, BPPV is often associated with a minor to severe blow to your head. Less common causes of BPPV include disorders that damage your inner ear or, rarely, damage that occurs during ear surgery or during prolonged positioning on your back. BPPV also has been associated with migraines. In many cases the doctors can’t figure out the cause.
Complications of BPPV:
Benign paroxysmal positional vertigo occurs most often in people age 60 and older, but can occur at any age. Aside from aging, there are no definite factors that may increase your risk of benign paroxysmal positional vertigo. However, a head injury or any other disorder of the balance organs of your ear may make you more susceptible to BPPV.
Although benign paroxysmal positional vertigo (BPPV) is uncomfortable, it rarely causes complications. In rare cases, if severe, persistent BPPV causes you to vomit frequently, you may be at risk of dehydration. The dizziness of BPPV can put you at greater risk of falling. It is more of a headache in going through the time to resolve the vertigo possibly affecting people in doing their regular activities of living for a week to several weeks. For some it never comes back but for many it does after several months depending on what the cause is.
TREATMENT
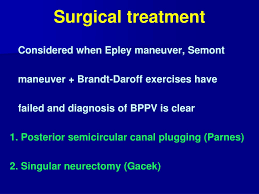
In all cases the doctor first has the patient (pt.) in their office and either through them or through physical therapy ordered by the M.D. after evaluating the pt with diagnosing the pt. with BPPV in treating the pt. using exercises which help in high percentages resolving the vertigo but continuing them when the vertigo is gone will do very little help unfortunately including it commonly comes back several weeks to months later and the exercises help more than. These exercises used are:
OFFICE TREATMENT OF BPPV are :
The Epley and Semont Maneuvers
There are two treatments of BPPV that are usually performed in the doctor’s office. Both treatments are very effective, with roughly an 80% cure rate, ( Herdman et al, 1993; Helminski et al, 2010). If your doctor is unfamiliar with these treatments, you can find a list of clinicians who have indicated that they are familiar with the maneuver from the Vestibular Disorders Association (VEDA) .
The maneuvers, named after their inventors, are both intended to move debris or “ear rocks” out of the sensitive part of the ear (posterior canal) to a less sensitive location. Each maneuver takes about 15 minutes to complete. The Semont maneuver (also called the “liberatory” maneuver) involves a procedure whereby the patient is rapidly moved from lying on one side to lying on the other (Levrat et al, 2003). It is a brisk maneuver that is not currently favored in the United States, but it is 90% effective after 4 treatment sessions. In our opinion, it is equivalent to the Epley maneuver as the head orientation with respect to gravity is very similar, omitting only ‘C’ from the figure to the right.
The Epley maneuver is also called the particle repositioning or canalith repositioning procedure. It was invented by Dr. John Epley, and is illustrated in figure 2. Click here for a low bandwidth animation. It involves sequential movement of the head into four positions, staying in each position for roughly 30 seconds. The recurrence rate for BPPV after these maneuvers is about 30 percent at one year, and in some instances a second treatment may be necessary.
When performing the Epley maneuver, caution is advised should neurological symptoms (for example, weakness, numbness, visual changes other than vertigo) occur. Occasionally such symptoms are caused by compression of the vertebral arteries (Sakaguchi et al, 2003), and if one persists for a long time, a stroke could occur. If the exercises are being performed without medical supervision, we advise stopping the exercises and consulting a physician. If the exercises are being supervised, given that the diagnosis of BPPV is well established, in most cases we modify the maneuver so that the positions are attained with body movements rather than head movements.
After either of these maneuvers, you should be prepared to follow the instructions of your doctor or physical therapist who should give you written instructions on them to take home with you, which are aimed at reducing the chance that debris might fall back into the sensitive back part of the ear. Not always the case.
What to expect from your doctor on your visit with vertigo:
A doctor who sees you for symptoms common to BPPV may ask a number of questions, such as:
- What are your symptoms, and when did you first notice them?
- Do your symptoms come and go? How often?
- How long do your symptoms last?
- Is one or both of your ears affected?
- Does anything in particular seem to trigger your symptoms, such as certain types of movement or activity?
- Do your symptoms include vision problems?
- Do your symptoms include nausea or vomiting?
- Do your symptoms include headache?
- Have you lost any hearing?
- Have you had any weakness, numbness or tingling in your arms or your legs?
- Have you had any difficulty talking or walking?
- Have you had chest pain?
- Are you being treated for any other medical conditions?
- What medications are you currently taking, including over-the-counter and prescription drugs as well as vitamins and supplements?