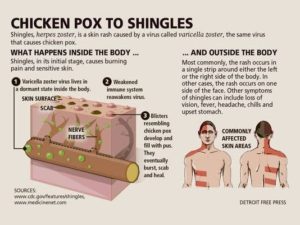
Shingles is a disease that affects your nerves. It can cause burning, shooting pain, tingling, and/or itching, as well as a rash and blisters.
You may recall having chickenpox as a child. Shingles is caused by the same virus, the varicella-zoster virus (VZV). After you recover from chickenpox, the virus continues to live in some of your nerve cells. It is usually inactive, so you don’t even know it’s there.
In fact, most adults live with VZV in their bodies and never get shingles. But, for about one in three adults, the virus will become active again. Instead of causing another case of chickenpox, it produces shingles. We do not totally understand what makes the virus go from inactive to active.
Having shingles doesn’t mean you have any other underlying disease.
Everyone who has had chickenpox has VZV in their body and is at risk for getting shingles. Right now, there is no way of knowing who will get the disease. But, some things make it more likely:
- Advanced age. The risk of getting shingles increases as you age. People may have a harder time fighting off infections as they get older. About half of all shingles cases are in adults age 60 or older. The chance of getting shingles becomes much greater by age 70.
- Trouble fighting infections. Your immune system is the part of your body that responds to infections. Age can affect your immune system. So can an HIV infection, cancer, cancer treatments, too much sun, or organ transplant drugs. Even stress or a cold can weaken your immune system for a short time. These all can put you at risk for shingles.
Can You Catch Shingles?
Shingles is not contagious. You can’t catch it from someone. But, you can catch chickenpox from someone with shingles. So, if you’ve never had chickenpox, try to stay away from anyone who has shingles.
If you have shingles, try to stay away from anyone who has not had chickenpox or who might have a weak immune system.
What Are the Symptoms of Shingles?
Usually, shingles develops only on one side of the body or face and in a small area rather than all over. The most common place for shingles is a band that goes around one side of your waistline.
Shingles on one side of the face 
How Long Does Shingles Last?
Most cases of shingles last three to five weeks. Shingles follows a pattern:
- The first sign is often burning or tingling pain; sometimes, it includes numbness or itching on one side of the body.
- Somewhere between one and five days after the tingling or burning feeling on the skin, a red rash will appear.
- A few days later, the rash will turn into fluid-filled blisters.
- About a week to 10 days after that, the blisters dry up and crust over.
- A couple of weeks later, the scabs clear up.
Most people get shingles only one time. But, it is possible to have it more than once.
Long-Term Pain and Other Lasting Problems
After the shingles rash goes away, some people may be left with ongoing pain called post-herpetic neuralgia or PHN. The pain is felt in the area where the rash had been. For some people, PHN is the longest lasting and worst part of shingles. The older you are when you get shingles, the greater your chance of developing PHN.
The PHN pain can cause depression, anxiety, sleeplessness, and weight loss. Some people with PHN find it hard to go about their daily activities, like dressing, cooking, and eating. Talk with your doctor if you have any of these problems.
There are medicines that may help with PHN. Steroids may lessen the pain and shorten the time you’re sick. Analgesics, antidepressants, and anticonvulsants may also reduce the pain. Usually, PHN will get better over time.
Some people have other problems that last after shingles has cleared up. For example, the blisters caused by shingles can become infected. They may also leave a scar. It is important to keep the area clean and try not to scratch the blisters. Your doctor can prescribe an antibiotic treatment if needed.
See your doctor right away if you notice blisters on your face—this is an urgent problem. Blisters near or in the eye can cause lasting eye damage or blindness. Hearing loss, a brief paralysis of the face, or, very rarely, swelling of the brain (encephalitis) can also occur.
Have a Rash? Go to the Doctor
If you think you might have shingles, talk to your doctor as soon as possible. It’s important to see your doctor no later than three days after the rash starts. The doctor will confirm whether or not you have shingles and can make a treatment plan. If you have a condition that weakens the immune system, the doctor may give you a shingles test. The shingles test can also help doctors diagnose shingles in people who don’t have a rash. Although there is no cure for shingles, early treatment with drugs that fight the virus can help the blisters dry up faster and limit severe pain. Shingles can often be treated at home. People with shingles rarely need to stay in a hospital.
Should You Get the Shingles Vaccine?
The shingles vaccine is safe and easy, and it may keep you from getting shingles and PHN. Healthy adults age 50 and older should get vaccinated with a shingles vaccine called Shingrix, which is given in two doses. Zostavax, a previous shingles vaccine, is no longer available in the United States.
You should try to get the second dose of Shingrix between two and six months after you get the first dose. If your doctor or pharmacist is out of Shingrix, you can use the Vaccine Finder to help find other providers who have Shingrix. You can also contact pharmacies in your area and ask to be put on a waiting list for Shingrix. If it’s been more than six months since you got the first dose, you should get the second dose as soon as possible. You don’t need to get a first dose again.
You should get Shingrix even if you have already had shingles, received Zostavax, or don’t remember having had chickenpox. However, you should not get a vaccine if you have a fever or illness, have a weakened immune system, or have had an allergic reaction to Shingrix. Check with your doctor if you are not sure what to do.
You can get the shingles vaccine at your doctor’s office and at some pharmacies. All Medicare Part D plans and most private health insurance plans will cover the cost.
What Can You Do About Shingles?
If you have shingles, here are some tips that might help you feel better:
- Get plenty of rest and eat well-balanced meals.
- Try simple exercises like stretching or walking. Check with your doctor before starting a new exercise routine.
- Apply a cool washcloth to your blisters to ease the pain and help dry the blisters.
- Do things that take your mind off your pain. For example, watch TV, read, talk with friends, listen to relaxing music, or work on a hobby you like.
- Avoid stress. It can make the pain worse.
- Wear loose-fitting, natural-fiber clothing.
- Take an oatmeal bath or use calamine lotion to see if it soothes your skin.
- Share your feelings about your pain with family and friends. Ask for their understanding.
Also, you can limit spreading the virus by:
- Keeping the rash covered
- Not touching or scratching the rash
- Washing your hands often
Most people have some of the following shingles symptoms:
- Burning, tingling, or numbness of the skin
- Feeling sick—chills, fever, upset stomach, or headache
- Fluid-filled blisters
- Skin that is sensitive to touch
- Mild itching to strong pain
Depending on where shingles develops, it could also cause symptoms like hiccups or even loss of vision.
For some people, the symptoms of shingles are mild. They might just have some itching. For others, shingles can cause intense pain that can be felt from the gentlest touch or breeze.
How Long Does Shingles Last?
Most cases of shingles last three to five weeks. Shingles follows a pattern:
- The first sign is often burning or tingling pain; sometimes, it includes numbness or itching on one side of the body.
- Somewhere between one and five days after the tingling or burning feeling on the skin, a red rash will appear.
- A few days later, the rash will turn into fluid-filled blisters.
- About a week to 10 days after that, the blisters dry up and crust over.
- A couple of weeks later, the scabs clear up.
Most people get shingles only one time. But, it is possible to have it more than once.