Center for disease prevention and control recommends the following:
Should you get screened for prostate cancer?
The answer is different for each man. If you are thinking about being screened, learn about the possible benefits and harms of screening, diagnosis, and treatment, and talk to your doctor about your personal risk factors.
What Is Prostate Cancer Screening?
Cancer screening means looking for cancer before it causes symptoms. The goal of screening for prostate cancer is to find cancer early that may spread if not treated.
There is no standard test to screen for prostate cancer. Two tests that are commonly used to screen for prostate cancer are—
- A blood test called a prostate specific antigen (PSA) test. PSA is a substance your prostate makes. This test measures the level of PSA in your blood. Your PSA level may be high if you have prostate cancer and for many other reasons, such as having an enlarged prostate, a prostate infection, or taking certain medicines.
- Digital rectal examination, when a health care provider inserts a gloved, lubricated finger into a man’s rectum to feel the prostate for anything abnormal, such as cancer.
Screening may find cancer that is likely to spread to other places in the body, so it can be treated before it spreads. This may lower the chance of death from prostate cancer in some men.
But most prostate cancers grow slowly and don’t cause any health problems. If a screening test finds a slow-growing cancer, it may cause you to worry, and lead to unneeded tests and treatments that can have serious side effects.
Also, a PSA test can be abnormal, but you don’t have prostate cancer. This is called a false positive result. A false positive PSA test result often leads to more unnecessary tests.
The only way to know if an abnormal test is due to cancer is to do a biopsy. A biopsy is when a small piece of tissue is removed from the prostate and looked at under a microscope to check for cancer. A prostate biopsy can cause pain, blood in the semen or ejaculate, and infection.
The most common treatments for localized (early-stage) prostate cancer are surgery to remove the prostate, radiation therapy, and active surveillance (getting tested regularly, and treating the cancer only if it grows or causes symptoms). Side effects from radiation therapy or surgery may include—
- Impotence.
- Loss of bladder control.
- Bowel problems.
Talk to Your Doctor
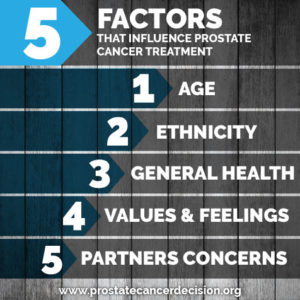
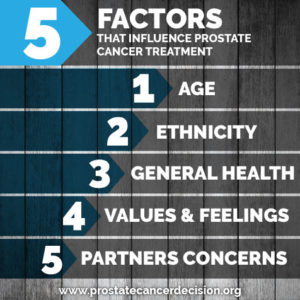
If you are thinking about being screened, you and your doctor should consider—
- If you have an increased risk of getting prostate cancer.
- If you have any health problems that may make it harder for you to be treated for prostate cancer if it is found, or that may make you less likely to benefit from screening.
- How you feel about the possible benefits and harms of screening, diagnosis, and treatment.