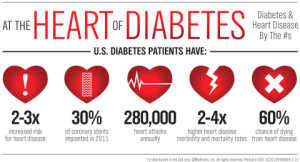
At least four complex processes, alone or combined, can lead to diabetic heart disease (DHD). They include coronary atherosclerosis; metabolic syndrome; insulin resistance in people who have type 2 diabetes; and the interaction of coronary heart disease (CHD), high blood pressure, and diabetes .
Researchers continue to study these processes because all of the details aren’t yet known.
Coronary Atherosclerosis
Atherosclerosis is a disease in which plaque builds up inside the arteries. The exact cause of atherosclerosis isn’t known. However, studies show that it is a slow, complex disease that may start in childhood. The disease develops faster as you age.
Coronary atherosclerosis may start when certain factors damage the inner layers of the coronary (heart) arteries. These factors include:
- Smoking
- High amounts of certain fats and cholesterol in the blood
- High blood pressure
- High amounts of sugar in the blood due to insulin resistance or diabetes
Plaque may begin to build up where the arteries are damaged. Over time, plaque hardens and narrows the arteries. This reduces the flow of oxygen-rich blood to your heart muscle.
Eventually, an area of plaque can rupture (break open). When this happens, blood cell fragments called platelets (PLATE-lets) stick to the site of the injury. They may clump together to form blood clots.
Blood clots narrow the coronary arteries even more. This limits the flow of oxygen-rich blood to your heart and may worsen angina (chest pain) or cause a heart attack.
Metabolic Syndrome
Metabolic syndrome is the name for a group of risk factors that raises your risk of both CHD and type 2 diabetes.
If you have three or more of the five metabolic risk factors, you have metabolic syndrome. The risk factors are:
- A large waistline (a waist measurement of 35 inches or more for women and 40 inches or more for men).
- A high triglyceride (tri-GLIH-seh-ride) level (or you’re on medicine to treat high triglycerides). Triglycerides are a type of fat found in the blood.
- A low HDL cholesterol level (or you’re on medicine to treat low HDL cholesterol). HDL sometimes is called “good” cholesterol. This is because it helps remove cholesterol from your arteries.
- High blood pressure (or you’re on medicine to treat high blood pressure).
- A high fasting blood sugar level (or you’re on medicine to treat high blood sugar).
It’s unclear whether these risk factors have a common cause or are mainly related by their combined effects on the heart.
Obesity seems to set the stage for metabolic syndrome. Obesity can cause harmful changes in body fats and how the body uses insulin.
Chronic (ongoing) inflammation also may occur in people who have metabolic syndrome. Inflammation is the body’s response to illness or injury. It may raise your risk of CHD and heart attack. Inflammation also may contribute to or worsen metabolic syndrome.
Research is ongoing to learn more about metabolic syndrome and how metabolic risk factors interact.
Insulin Resistance in People Who Have Type 2 Diabetes
Type 2 diabetes usually begins with insulin resistance. Insulin resistance means that the body can’t properly use the insulin it makes.
People who have type 2 diabetes and insulin resistance have higher levels of substances in the blood that cause blood clots. Blood clots can block the coronary arteries and cause a heart attack or even death.
The Interaction of Coronary Heart Disease, High Blood Pressure, and Diabetes
Each of these risk factors alone can damage the heart. CHD reduces the flow of oxygen-rich blood to your heart muscle. High blood pressure and diabetes may cause harmful changes in the structure and function of the heart.
Having CHD, high blood pressure, and diabetes is even more harmful to the heart. Together, these conditions can severely damage the heart muscle. As a result, the heart has to work harder than normal. Over time, the heart weakens and isn’t able to pump enough blood to meet the body’s needs. This condition is called heart failure.
As the heart weakens, the body may release proteins and other substances into the blood. These proteins and substances also can harm the heart and worsen heart failure.