Diabetes is becoming more common in the United States. From 1980 through 2011, the number of Americans with diagnosed diabetes has more than tripled (from 5.6 million to 20.9 million). Do you know how much it is costing in our country?
What is diabetes?
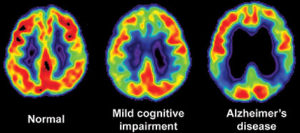
Diabetes is a group of diseases marked by high levels of blood glucose resulting from defects in insulin production, insulin action, or both. Diabetes can lead to serious complications and premature death, but people with diabetes, working together with their support network and their health care providers, can take steps to control the disease and lower the risk of complications.
There are 2 types:
Type 1 diabetes was previously called insulin-dependent mellitus (IDDM) or juvenile-onset diabetes. This type of diabetes happens when the immune system ends up destroying beta cells in the body that come from our pancreas and they are the only cells in the human body that make the hormone INSULIN the regulates your glucose. Insulin allows glucose to transfer into the cells and tissues of our body to give them their energy to do their job in the body and nutrition to work properly=sugar-glucose. To live with this diabetes the person must have their insulin delivered by injection or a pump. This form of diabetes usually occurs in children or young adults but can occur at any age.
Type 2 diabetes was called non-insulin dependent diabetes mellitus (NIDDM) or adult-onset diabetes. In adults, type 2 diabetes accounts for about 90-95% of all diagnosed cases of diabetes. It usually begins as insulin resistance, a disease in which the cells do not use insulin properly due to the pancreas not making enough or the pancreas not secreting the correct form o of insulin to do its function. Ending line the insulin isn’t working properly. As the need for insulin rises, the pancreas gradually loses its ability to produce it.
Type 2 diabetes is associated with older age, OBESITY, family history of diabetes, history of gestational diabetes, impaired glucose metabolism, physical inactivity and race/ethnicity.
Gestational diabetes is a form of glucose intolerance diagnosed during pregnancy. Gestational diabetes occurs more frequently among African Americans, Hispanic/Latino Americans, and American Indians. It is also more common among obese women and women with a family history of diabetes. During pregnancy, gestational diabetes requires treatment to optimize maternal blood glucose levels to lessen the risk of complications in the infant.
Other types of diabetes result from specific genetic conditions (such as maturity-onset diabetes of youth), surgery, medications, infections, pancreatic disease, and other illnesses. Such types of diabetes account for 1% to 5% of all diagnosed cases.
Treating diabetes
Diet, insulin, and oral medication to lower blood glucose levels are the foundation of diabetes treatment and management. Patient education and self-care practices are also important aspects of disease management that help people with diabetes lead normal lives.
- To survive, people with type 1 diabetes must have insulin delivered by injection or a pump.
- Many people with type 2 diabetes can control their blood glucose by following a healthy meal plan and exercise program, losing excess weight, and taking oral medication. Medications for each individual with diabetes will often change during the course of the disease. Some people with type 2 diabetes may also need insulin to control their blood glucose.
Self-management education or training is a key step in improving health outcomes and quality of life. It focuses on self-care behaviors, such as healthy eating, being active, and monitoring blood sugar.
Criteria for the diagnosis of diabetes:
- A fasting blood sugar level ≥126 milligrams per deciliter (mg/dL) after an overnight fast, which is just taking the finger stick right when you wake up before breakfast OR
- A 2-hour blood sugar level ≥200 mg/dL after a 2-hour oral glucose tolerance test (OGTT), OR
- An A1c level ≥6.5%. (The A1C test is a simple lab test that measures average blood glucose levels over the past 3 months. A small blood sample to check your A1C can be taken at any time of the day=simply a blood test)
- Pretty simple isn’t it.
Diabetes is not only common and serious; it is also VERY COSTLY! Let us take a look:
The cost of treating diabetes is staggering. According to the American Diabetes Association, the annual cost of diabetes in medical expenses and lost productivity rose for $98 billion in 1997 to $132 billion in $2002 to $174 billion in 2007.
One out of every 5 U.S. federal health care dollars is spent treating people with diabetes. The average yearly health care costs for a person without diabetes is 2,560 dollars; for a person with diabetes that figure soars to $11,744. Much of the human and financial costs can be avoided with proven diabetes prevention and management steps.
Turn into PART 2 tomorrow and learn what the symptoms and complications are of Diabetes with how to decrease your odds of getting Diabetes with knowing what measures to take to better control your Diabetes, with your doctor’s approval.
REFERENCES for Part 1 and Part 2 :
- Center for Disease (CDC) – “National Diabetes Fact Sheet”
- NYS Dept. of Health –Diabetes
- Diabetic Neuropathy.org “All about diabetic neuropathy&nerve damage caused by Diabetes.”Copyright 02–04.
- NIDDK “National Institute of Diabetes and Digestive and Kidney Diseases”
- National Diabetes Information Clearinghouse (NIDC) – U.S. Department of Health and Human Services. “Preventing Diabetes Problems: What you need to know”