One of the most emotionally complex and difficult things a person can experience is taking care of an elderly parent. I unfortunately had to spend time tending to my aging, dying father, and thought I’d pass along these several points, each of which I found to be significantly helpful during then and now with caring for my mom in the phase of my own life.
- Accept that things have changed. When a parent starts in any way depending upon their child, a world has turned upside down. Be prepared for that radically new paradigm. Old roles may not apply; old methodologies may not apply; old emotions may not apply. Be prepared to work from — and write — a whole new script. With my father things happened to quick and I had to think medical as a RN (my profession). I knew what to ask when he was in the hospital and when to stop chemo and ask for hospice and how to go about with my mom when she was telling me all these different people said this and that. I just had to say mom the MD is the bible (with my mom being severely catholic) and with all the money you pay him he is the best candidate to listen to in what should be done for the best optimal care not a priest or catholic friend or a child not in the medical profession. She was cooperative in doing this where I made the call being in one room of my mother’s and father’s home and my mom in another room. I called the MD introducing myself and what my profession was with several years being a RN. I stated to the MD “If this was your father what would you recommend at this time?” (with knowing the answer already). The MD stated I would stop the chemo. I knew the next option was hospice and told the md please get my father under hospice with than allowing my mother to take over the conversation from there and hung up. This gave my mother independence now in finalizing the hospice care.
- Take it slowly. Taking care of an elderly parent is generally a marathon, not a sprint. Don’t rush it. You and they both are in uncharted territory. Let the process reveal itself to you; to the degree that you can, let whatever happens unfold organically. As much as you lead what’s happening, follow it.
- Expect nothing emotionally. At the end phase of their life, your parent might open up to you emotionally and spiritually; they might express for you the love that, for whatever reason, they haven’t before. But they also might not do that; your parent might even more tenaciously cling to their crazy. If as you care for your aging parent you bond with them in a new and deeper way, of course that’s fantastic. But going into caring for them expecting or even hoping for that to happen is to wade into dangerous waters. Better to have no expectations and be surprised, than to have your hopes dashed.
- Expect their anger. When you start taking care of your parent, they lose the one thing they’ve always had in relationship to you: authority. That’s not going to be easy for them to give up. Expect them, in one way or another, to lash out about that loss.
- Give them their autonomy. Insofar as you can, offer your parent options instead of orders. It’s important for them to continue to feel as if they, and not you, are running their lives. Let them decide everything they can about their own care and situation.
- Ask their advice. A great way to show your parent love and respect — and, especially, to affirm for them that they are still of true value to you — is to sincerely ask them for advice about something going on in your life.
- Separate their emotional dysfunction from their cognitive dysfunction. Insofar as you can, through your conversations and interactions with your parent, learn to distinguish between their emotional and cognitive dysfunction. The patterns of your parent’s emotional dysfunctions will probably be familiar to you; those, you’ll know how to deal with. But their cognitive dysfunctioning will probably be new to you. Track it; react to it gingerly; discuss it with your parent’s health care providers. Mostly, just be aware that it’s new, and so demands a new kind of response. This is a part of the process where it’s good to remember point No. 2.
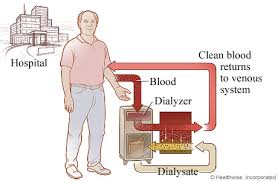
- Love your health care providers. During this phase of your life, you don’t have better friends than those helping you care for your parent. Cleaning person, social worker, physical therapist, nurse, doctor, caring neighbor — treat well each and every person who plays any role whatsoever in caring for your parent. When they think of your parent, you want everyone involved in their care to have good, positive thoughts; you want them to want to care well for your mom or dad. Steady kindness, and little gifts here and there, can go a long way toward ensuring that’s how they feel.
- Depend upon your spouse. You may find that your parent is more comfortable relating to your spouse than to you. Though that can certainly hurt your feelings, don’t let it. It’s simply because your parent doesn’t share with your spouse all the baggage they do with you; mainly, they’ve never been the dominate force in your spouse’s life. Your spouse and your parent are peers to a degree that you and your parent can never be. Let that work for you. Depend upon your spouse to be as instrumental in the care of your parent as he or she wants to be.
- Protect your buttons. No one in this world knows your emotional buttons like your mom or dad does. Surround those buttons with titanium cases and lock them away where your parent couldn’t find them with a Rorschach test. Unless he or she is an extraordinarily loving and mature person, your parent is bound to at least once try to push your buttons, if only to establish their erstwhile dominance over you. Don’t let them do it. You might owe them your care, but you don’t owe them your emotional well-being. With your parent, let “No buttons for you!” be your motto.
- Prepare for sibling insanity. Expect the worst from your sibling(s). For perfectly understandable reasons, many people go positively bonkers when their parents start to die. Money, childhood mementos, furniture and possessions from the family house, money, diversified assets, money, the will… you get the idea. Prepare for the coming crazy. Do not participate in it yourself. Insofar as you must, of course protect yourself. But no amount of money on earth is worth your dignity.
- Take care of yourself . It’s so easy to surrender to the care of your aging parent more of your life than you should. But you serve well neither yourself nor them if you fail to take walks; to stretch out; to eat right; to make sure you spend quality time away from them. Make taking time to rejuvenate yourself as critical a part of your care routine for your parent as you do cooking their meals or making sure they take their meds. Your life still needs to be about you.
- Talk to a friend. If you have a friend with whom you can regularly meet and talk, or even chat with on the phone, do it. During this time the input and love of a friend is invaluable to you. Sharing what you’re going through with someone not immediately involved with it can be like a life preserver when you’re bobbing in the ocean. As soon as you get involved with tending to your parent, call your best friend, and tell them that you’re going to be depending upon them to do what friends do best: care, and listen.
- Have fun. One of the things we most need in life is the one thing we most readily jettison once we begin caring for an elderly parent: fun. Fun! Have some! Have lots! Rent a Marx Brothers movie. Wear a goofy hat. Make your parent wear a goofy hat — when they’re sleeping, Whatever it takes. But remember: A day without fun is like a day where you almost go to jail for pushing your old mom or dad down a stairwell. Whenever, wherever and however you can, truly enjoy.
- Pray or meditate. Life doesn’t offer a lot more emotionally salient or complex than caring for an aging parent. Accordingly, then, open yourself up to God, whatever that might mean to you. Be sure to with some regularly get down on your knees, or sit comfortably in a quiet place; close your eyes; breathe deeply and slowly; and wait to come over you the peace that surpasses understanding. What you’re undergoing with your parent right now is bigger than you, your parent, or anyone else involved. Do not fail to avail yourself of the great and mighty source from whose perspective it has all, already, been resolved..