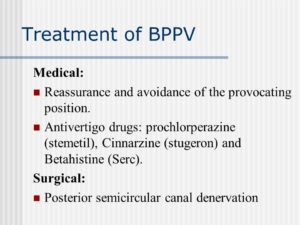
Reassurance and avoidance of the provocating position. Antivertigo drugs: prochlorperazine (stemetil), Cinnarzine (stugeron) and Betahistine (Serc). Surgical: Posterior semicircular canal denervation.
TREATMENT
In all cases the doctor first has the patient (pt.) in their office and either through them or through physical therapy ordered by the M.D. after evaluating the pt with diagnosing the pt. with BPPV in treating the pt. using exercises which help in high percentages resolving the vertigo but continuing them when the vertigo is gone will do very little help unfortunately including it commonly comes back several weeks to months later and the exercises help more than. These exercises used are:
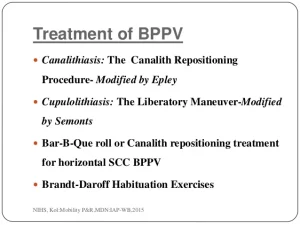
OFFICE TREATMENT OF BPPV: The Epley and Semont Maneuvers
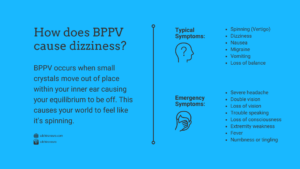
There are two treatments of BPPV that are usually performed in the doctor’s office. Both treatments are very effective, with roughly an 80% cure rate, ( Herdman et al, 1993; Helminski et al, 2010). If your doctor is unfamiliar with these treatments, you can find a list of clinicians who have indicated that they are familiar with the maneuver from the Vestibular Disorders Association (VEDA) .
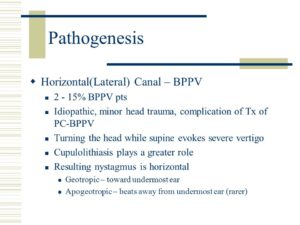
The maneuvers, named after their inventors, are both intended to move debris or “ear rocks” out of the sensitive part of the ear (posterior canal) to a less sensitive location. Each maneuver takes about 15 minutes to complete. The Semont maneuver (also called the “liberatory” maneuver) involves a procedure whereby the patient is rapidly moved from lying on one side to lying on the other (Levrat et al, 2003). It is a brisk maneuver that is not currently favored in the United States, but it is 90% effective after 4 treatment sessions. In our opinion, it is equivalent to the Epley maneuver as the head orientation with respect to gravity is very similar, omitting only ‘C’ from the figure to the right.
The Epley maneuver is also called the particle repositioning or canalith repositioning procedure. It was invented by Dr. John Epley. It involves sequential movement of the head into four positions, staying in each position for roughly 30 seconds. The recurrence rate for BPPV after these maneuvers is about 30 percent at one year, and in some instances a second treatment may be necessary.
When performing the Epley maneuver, caution is advised should neurological symptoms (for example, weakness, numbness, visual changes other than vertigo) occur. Occasionally such symptoms are caused by compression of the vertebral arteries (Sakaguchi et al, 2003), and if one persists for a long time, a stroke could occur. If the exercises are being performed without medical supervision, we advise stopping the exercises and consulting a physician. If the exercises are being supervised, given that the diagnosis of BPPV is well established, in most cases we modify the maneuver so that the positions are attained with body movements rather than head movements.
After either of these maneuvers, you should be prepared to follow the instructions of your doctor or physical therapist who should give you written instructions on them to take home with you, which are aimed at reducing the chance that debris might fall back into the sensitive back part of the ear. Not always the case.
What to expect from your doctor on your visit with vertigo
A doctor who sees you for symptoms common to BPPV may ask a number of questions, such as:
- What are your symptoms, and when did you first notice them?
- Do your symptoms come and go? How often?
- How long do your symptoms last?
- Is one or both of your ears affected?
- Does anything in particular seem to trigger your symptoms, such as certain types of movement or activity?
- Do your symptoms include vision problems?
- Do your symptoms include nausea or vomiting?
- Do your symptoms include headache?
- Have you lost any hearing?
- Have you had any weakness, numbness or tingling in your arms or your legs?
- Have you had any difficulty talking or walking?
- Have you had chest pain?
- Are you being treated for any other medical conditions?
- What medications are you currently taking, including over-the-counter and prescription drugs as well as vitamins and supplements?
Need assistance in where to go for help treatment on surgery in the hospitat for benign posterior paroxysmal vertigo? Than tune in tomorrow to Part IV.

 ZZXdcfvgbhnjmk,.
ZZXdcfvgbhnjmk,.