A particular cell known as the Reed-Sternberg cell is found in the biopsies. This cell is not usually found in other lymphomas, therefore they are called non Hodgkins lymphoma. This may not seem a very big difference, but it is important because the treatment for Hodgkins and non Hodgkins lymphomas can be very different.
Although the diseases may sound similar, there is a lot of difference between Hodgkin and non-Hodgkin lymphoma.
Both Hodgkin and non-Hodgkin lymphoma are malignancies of a family of white blood cells known as lymphocytes, which help the body fight off infections and other diseases.
Both Hodgkin’s lymphoma and non-Hodgkin’s lymphoma are lymphomas — a type of cancer that begins in a subset of white blood cells and these are called lymphocytes. Lymphocytes are an integral part of your immune system, which protects you from germs.
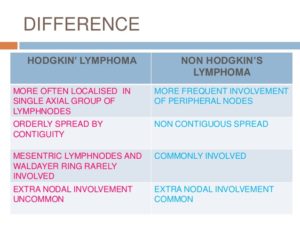
The main difference between Hodgkin’s lymphoma and non-Hodgkin’s lymphoma is in the specific lymphocyte each involves but also it includes:
| Hodgkin lymphoma | Non-Hodgkin lymphoma |
|---|---|
| Thirty-two percent of patients diagnosed with Hodgkin lymphoma are 20-34 years old. The median age of a patient diagnosed with the disease is 39. | Seventy-five percent of patients diagnosed with Hodgkin lymphoma 55 or older. The median age of a patient diagnosed with the disease is 66. |
| Hodgkin lymphoma is rare, accounting for about .5 percent of all new cancers diagnosed. An estimated 8,500 cases were diagnosed in 2016. | Non-Hodgkin lymphoma is the seventh most diagnosed cancer, accounting for an estimated 72,500 cases in 2016. |
| More than 86 percent of patients diagnosed with Hodgkin lymphoma survive five years or more. | About 70 percent of patients diagnosed with non-Hodgkin lymphoma survive five years or more. |
| There are six varieties of Hodgkin lymphoma. The most common forms are nodular sclerosis classical Hodgkin lymphoma and mixed cellularity classical Hodgkin lymphoma. They account for about 90 percent of all cases. | There are more than 61 types and subtypes of non-Hodgkin lymphoma. B-cell lymphomas account for 85 percent of all cases. Diffuse large B-cell lymphoma is the most common form on non-Hodgkin lymphoma. |
Sources: National Cancer Institute and Lymphoma Research Foundation 2016
Hodgkin lymphoma is marked by the presence of Reed-Sternberg cells, which are mature B cells that have become malignant, are unusually large, and carry more than one nucleus. The first sign of the disease is often the appearance of enlarged lymph nodes. Non-Hodgkin lymphoma, by contrast, can be derived from B cells or T cells and can arise in the lymph nodes as well as other organs. (B cells and T cells play different roles in the body’s immune response to disease.)
The the Mayo Clinic it states both diseases are relatively rare, but non-Hodgkin lymphoma is more common in the United States, with more than 70,000 new cases diagnosed each year, compared to about 8,000 for Hodgkin lymphoma. The median age of patients with non-Hodgkin lymphoma is 60, but it occurs in all age groups. Hodgkin lymphoma most often occurs in people ages 15 to 24 and in people over 60. There are more than 60 distinct types of non-Hodgkin lymphoma, whereas Hodgkin lymphoma is a more homogeneous disease.
The two forms of lymphoma are marked by a painless swelling of the lymph nodes. Hodgkin lymphomas are more likely to arise in the upper portion of the body (the neck, underarms, or chest). Non-Hodgkin lymphoma can arise in lymph nodes throughout the body, but can also arise in normal organs. Patients with either type can have symptoms such as weight loss, fevers, and night sweats.
The diseases often follow different courses of progression. Hodgkin lymphoma tends to progress in an orderly fashion, moving from one group of lymph nodes to the next, and is often diagnosed before it reaches an advanced stage. Most patients with non-Hodgkin lymphoma are diagnosed at a more advanced stage.
Treatments for lymphoma vary depending on the type of disease, its aggressiveness, and location, along with the age and general health of the patient. As a general rule, however, Hodgkin lymphoma is considered one of the most treatable cancers, with more than 90 percent of patients surviving more than five years. Survival rates for patients with non-Hodgkin lymphoma tend to be lower, but for certain types of the disease, the survival rates are similar to those of patients with Hodgkin lymphoma.
A doctor can tell the difference between Hodgkin’s lymphoma and non-Hodgkin’s lymphoma by examining the cancer cells under a microscope. If in examining the cells, the doctor detects the presence of a specific type of abnormal cell called a Reed-Sternberg cell, the lymphoma is classified as Hodgkin’s. If the Reed-Sternberg cell is not present, the lymphoma is classified as non-Hodgkin’s.
Many subtypes of lymphoma exist, and your doctor will use laboratory tests to examine a sample of your lymphoma cells to determine your specific subtype. Expect to wait a few days to receive results from these specialized tests.
Your type of lymphoma helps your doctor determine your prognosis and your treatment options. The types of lymphoma have very different disease courses and treatment choices, so an accurate diagnosis is an integral part of getting the care you need.
How both Hodgkin’s and Non-Hodgkin’s Disease are diagnosed:
- Physical exam. Your doctor checks for swollen lymph nodes, including in your neck, underarm and groin, as well as for a swollen spleen or liver.
- Blood and urine tests. Blood and urine tests may help rule out an infection or other disease. A sample of your blood is examined in a lab to see if anything in your blood indicates the possibility of cancer (in both of these diseases particularly the WBCs).
- Imaging tests. Your doctor may recommend imaging tests to look for tumors in your body. Tests may include X-ray, CT, MRI and positron emission tomography (PET).
- Lymph node test. Your doctor may recommend a lymph node biopsy procedure to remove all or part of a lymph node for laboratory testing. Analyzing lymph node tissue in a lab may reveal whether you have non-Hodgkin’s lymphoma and, if so, which type. Your doctor may recommend a lymph node biopsy procedure to remove a lymph node for laboratory testing. He or she will diagnose classical Hodgkin’s lymphoma if abnormal cells called Reed-Sternberg cells are found within the lymph node.
- Bone marrow test. A bone marrow biopsy and aspiration procedure involves inserting a needle into your hipbone to remove a sample of bone marrow. The sample is analyzed to look for non-Hodgkin’s lymphoma cells to look for non-Hodgkin’s lymphoma cells or to look for non-Hodgkin’s lymphoma cells. This test is done on numerous types of cancer patients in helping to diagnose the cancer they have.