The symptoms indicating a Myocardial Infarction or Heart Attack:
Chest pain or discomfort-Pain or discomfort in the jaw, neck or back
Pain or discomfort in the arms or shoulders
Shortness of breath
Feeling very tired or lightheaded or faint-Remember for many which is more men asymptomatic in many cases other than possibly feeling just weak or faint.
Nausea or vomiting
**If any the symptoms are present call 911!**
The sooner you get the pt to the ER the better; especially if no defibrillator is present where the person having a MI is located and if he or she needs it!! Time matters including what treatment is needed! The sooner the treatment the better in many cases regarding the ending result of the person’s condition. Since the sooner the treatment the better where in a lot of cases the ending result for the pt having an MI is worse due to prolonging medical treatment. An MI is scarring of the heart tissue where the MI occurred due to lack of oxygen to that area of the heart and is not reversible! The sooner the treatment the less damage to the heart in many cases with better results!
It’s the holiday season—cardiac patients not careful in eating but indulging in junk food may put you at high risk for a bomb to go off in the heart=heart attack.
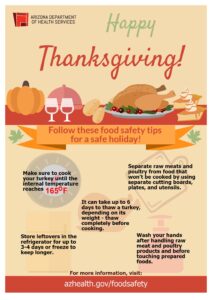
While colder weather may play a role, studies have shown that the spike in heart events during the holiday season occurs even in It’s no secret that holiday celebrations offer many temptations to overindulge. Many holiday foods are high in saturated fats or sodium. Overindulgence in these foods can increase cholesterol levels or blood pressure, making it more difficult for blood to flow through arteries and upping the chance of a blockage. What you may not know is that eating a heavy holiday meal may affect you even after you’ve pushed away from the table. “Research shows that anyone with coronary-artery disease or high cholesterol has a heightened risk for heart attack for up to one day after eating a heavy meal,” said Mittleman. Mittleman participated in a study, “Heavy Meals May Trigger Heart Attacks,” led by Francisco Lopez-Jimenez, MD, currently the Director of the Cardio-metabolic Program at the Mayo Clinic. This study, which focused on nearly 2,000 former heart attack patients, found that 10 percent of them suffered a coronary within 26 hours of eating a heavy meal.
“People often change their eating habits during the holidays,” said Dr. Anne Riley, a cardiologist at BIDMC. “For those with congestive heart failure [CHF], salty foods can cause fluid retention and high blood pressure, which place added stress on an already weakened heart.”
Your heart may leap with delight on the couch after Thanksgiving or at the electronic gizmo or emerald bracelet that you’ve just unwrapped from under the Christmas tree. But you can’t say the same for that nasty holiday surprise known as the “Happy Thanksgining” or “Merry Christmas coronary” or “Happy Hanukkah heart attack.”
For many years, researchers have been intrigued by a disturbing pattern: Deadly heart attacks increase during the winter holiday season. One study even found distinct spikes around Christmas and New Year’s Day.
Recommended Related to Heart Health
Read Amazing Facts About Heart Health and Heart Disease:
You can feel your heart thudding away every time you put your hand to your chest, but do you have any idea what’s really going on in there or what keeps your heart ticking as it should? WebMD the Magazine asked Richard Krasuski, MD, director of Adult Congenital Heart Disease Services and a staff cardiologist at the Cleveland Clinic, to help explain some amazing and little-known facts about the human heart.
“We certainly know that there are certain risk factors for coronary artery disease. There’s obviously smoking, hypertension, dyslipidemia [high cholesterol], diabetes, lack of exercise, and age,” says Robert A. Kloner, MD, PhD, a researcher at Good Samaritan Hospital in Los Angeles and a professor at the Keck School of Medicine at the University of Southern California.
“But we’re also learning that there are certain triggers for cardiovascular events,” he adds, “including time of the year and seasons. If we can get a true handle on the seasonal variation, we could knock down death from coronary disease.”
Coronary artery disease stems from atherosclerosis, a condition in which fatty plaques narrow the arteries to the heart. When a plaque ruptures, it can trigger a blood clot that leads to a heart attack.
In a national 2004 study published in Circulation, researchers at the University of California, San Diego, and Tufts University School of Medicine examined 53 million U.S. death certificates from 1973 to 2001. They discovered an overall increase of 5% more heart-related deaths during the holiday season. When researchers looked at individual years, they found varying increases in cardiac deaths for every holiday period they studied, except two.
Doctors have long known that cold weather is hard on the heart. Blood vessels constrict, which raises blood pressure. Blood also clots more readily. Frigid temperatures increase strain on the heart, and too much physical exertion can worsen the burden and trigger a heart attack. For example, doctors have treated many patients whose heart attacks followed strenuous snow shoveling.
Not to put a damper on holiday frivolity, but heart attacks increase during winter. For one reason, cold weather is tough on the heart. Blood vessels constrict, which causes blood pressure to rise. Additionally, blood clots more easily. (I’m getting this info, by the way, from the boldface link a sentence or two ago).
“People tend to consume much more fat, salt, sugar, and alcohol during the holiday season,”. “Also, people tend to be less active due to the cooler weather. Overindulgence of food and alcohol along with inactivity raises the blood pressure and cholesterol levels. These risk factors combined increase your chances of having congestive heart failure, a stroke, or even a heart attack.” says Roberto Wayhs, MD, chief of cardiology at Methodist Charlton Medical Center.
To put a stop to that, or at least decrease your chances, he offers these tips:
Limit foods and beverages that are salty and/or rich. Blood pressure tends to go up the more salt you intake. Rich and sugary foods raise blood sugar levels.
Be consistent in taking your daily medications. You need them at all times of the year to maintain good health.
Get enough sleep. Sleep loss is related to weight gain, which also can affect the heart. Aim for at least seven hours.
Control your stress. “Holiday sadness adds stress,” Wayhs says. “Don’t be afraid to seek professional help if you need it.”
Limit alcohol intake. “High alcohol intake has been linked to irregular and rapid heartbeats (atrial fibrillation) and congestive heart failure,” says Dr. Wayhs.
Maintain your normal exercise routine. “Don’t place your healthy habits on the back burner,” he says.
If you don’t have time for your usual workouts, try a shorter one.
Oh and, of course, stop smoking. But you knew that already.