Working of the heart:
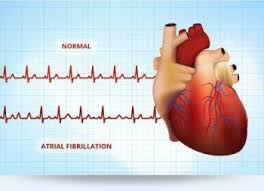
To easily identify atrial fibrillation with RVR, it is vital to understand the working of the heart. The atrium or atria (plural) is the upper chamber of the heart, bigger in size compared to the lower chambers known as the ventricles. The atria function by gathering blood as it flows into the heart and shrinking to forward the blood into the ventricles. At the very moment, the smaller ventricle must shrink to forward the blood to all parts of the body. This rhythm of blood flow creates a heart signature voice referred to as the Sinus rhythm. It is important that the sinus rhythm is synchronized so that the atrium does not send blood into the ventricle out of cue. To achieve this, an electric signal is generated to ensure the atrium contracts. When this signal short circuits (bypasses) the atrium, atrial fibrillation with RVR occurs, and the atrium is seen to vibrate just like jelly on a flat surface.
Atrial fib with RVR refers to atrial fibrillation with rapid ventricular rate. Usually the heart is like clockwork, the top (collecting) chambers beat then the bottom (main pumping) chambers sense this and also beat, and so on, in a nice regular fashion just like a clock ticking second after second. Usually the heart beats at about 60-80 beats per minute.
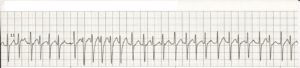
In atrial fibrillation the top chamber basically goes crazy often firing off over 400 beats per minute! Atrial fibrillation with RVR (Rapid Ventricular Response) is a heart condition caused by irregular electrical activity that results in irregular contractions of the 2 top heart chambers fibrillating. This means the heart (atriums), shakes with a rapid tremulous movement or makes fine irregular twitching movements, generally referred to as fibrillating causing little control in the heart output of blood by the heart but the lower chambers called the ventricles take over.
These bottom chambers don’t allow all those impulses through but it does let every second or third one through. This can give a heart rate of 100-180 beats per minute at rest, still too many beats, known as Afib with RVR, leading to symptoms and problems with heart function. Afib does not necessarily lead to Afib with RVR however, Afib can be rate controlled, sometimes naturally, sometimes using medications and sometimes requiring procedures as discussed below.
In most people with AFib although symptoms can sometimes be unpleasant it is generally not harmful as long as the afib is controlled, meaning the heart in the afib rhythm with the pulse under 100. The main concern is stroke, but that can be treated with the use of blood thinning medications in people at risk. In Afib with RVR, basically the heart is beating too fast. Of course palpitations are the most common symptom. Other symptoms of AFib with RVR may include dizziness, lack of energy, exercise intolerance and shortness of breath. If Afib with RVR goes on for too long then this may result in heart failure and of course worsening of existing heart failure. Control of the heart rate in patients with Afib with RVR often causes these symptoms to improve, again meaning the HR is under 100 with the heart rhythm in afib.
A major indication of atrial fibrillation with RVR is a very rapid heartbeat rate, although some patients are known to have the condition without showing symptoms. Atrial fibrillation with RVR may occur when cardiac muscle cells overcome their intrinsic pacemaker’s signals and fire rapidly differently from their normal pattern spreading the abnormal activity to the ventricles. The rapid heart rate can strain the heart, developing a situation referred to as Tachycardia (meaning a pulse greater than 100). Atrial fibrillation with RVR can be detected from the various symptoms though it is important to remember that some patients have experienced the condition without symptoms.
Symptoms:
Some of the symptoms of this disease include heart palpitations (described as unnoticed skipped beats or skipped beats noticed from experienced dizziness or difficulty in breathing), shortness of breath when lying flat (orthopnea), shortness of breath (dyspnea after exertion) sudden onset of short breath during the night (also called paroxysmal nocturnal dyspnea) and gradual swelling of lower extremities. As a result of inadequate blood flow, some patients complain of light headedness and may feel like they are about to faint, a condition referred to as presyncope and may actually lose consciousness (syncope). Some patients experience respiratory distress that results in them appearing blue. A close examination of jugular veins usually reveals elevated pressure in some patients (jugular venous distention). When some patients are subjected to lung examinations, crackles and rales may be observed pointing to possible lung edema.