Continuation of Types of Skin Cancer:
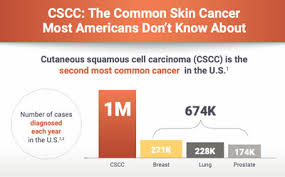
3-Squamous cell carcinoma – SCC
Squamous cell carcinoma is the second most common form of skin cancer in the United States. It accounts for about 15 percent of all skin cancers. It is caused due to over production of skin cells. Squamous cell carcinoma of the skin is caused by DNA damage that leads to abnormal changes (mutations) in the squamous cells in the outermost layer of skin. This cancer is common (More than 200,000 cases per year in US). The majority of squamous cell skin cancers are easily and successfully treated with current therapies.
Knowing the causes, risk factors and warning signs can help you detect them early, when they are easiest to treat and cure.
The risk factors of SCC:
–UV exposure from the sun or indoor tanning.
-History of skin cancer, including squamous cell carcinoma (SCC) or melanoma
– Age over 50: Most BCCs appear in people over age 50.
-Fair skin: People with fair skin have an increased risk.
Warning Signs can help with early detection and treatment this can be successfully removed without complications. Look out for any new, changing or unusual skin growths, so you can spot skin cancers like BCC when they are easiest to treat and cure.
IT’S A FACT, Squamous cell carcinoma is considered more aggressive than basal cell carcinoma. If squamous cell carcinoma does spread to internal organs it can be life threatening. The quicker the treatment when SCC is in the one layer of skin only the better the results. The primary symptom to look out for with SCC is a growing bump or lesion on the skin which has a rough scaly surface or flat red patches.
Treatments for SCC:
If the skin cancer is small, not deep into the skin, called superficial, and has a low risk of spreading, less-invasive treatment choices include:
- Curettage and electrodessication. This treatment involves removing the top of the skin cancer with a scraping tool called a curet. Then an electric needle is used to sear the base of the cancer.
- Laser therapy. This treatment uses an intense beam of light to destroy growths. There’s usually little damage to nearby tissue. And there’s a reduced risk of bleeding, swelling and scarring.
- Freezing. This treatment, called cryosurgery, involves freezing cancer cells with liquid nitrogen. Freezing might be done after using a scraping tool, called a curet, to remove the surface of the skin cancer.
- Photodynamic therapy. During photodynamic therapy, a liquid medicine that makes the cancer cells sensitive to light is applied to the skin. Later, a light that destroys the skin cancer cells is shined on the area. This treatment might be used with surgery or other treatments.
Treatments for larger skin cancers:
More-invasive treatments might be recommended for larger squamous cell carcinomas and those that go deeper into the skin. Options might include:
- Simple excision. This involves cutting out the cancer and a margin of healthy skin around it. Sometimes more skin around the tumor is removed, called a wide excision.
- Mohs surgery. Mohs surgery involves removing the cancer layer by layer and looking at each layer under the microscope until no cancer cells are left. This allows the surgeon to remove the whole growth without taking too much of the healthy skin around it.
- Radiation therapy. Radiation therapy uses powerful energy beams to kill cancer cells. Radiation therapy is sometimes used after surgery when there is an increased risk that the cancer might return. It also might be an option for people who can’t have or don’t want surgery.
Treatments for skin cancer that spreads past the skin:
When squamous cell carcinoma spreads to other parts of the body, medicines might be recommended, including:
- Chemotherapy. Chemotherapy uses strong medicines to kill cancer cells. If squamous cell carcinoma spreads to the lymph nodes or other parts of the body, chemotherapy can be used alone or with other treatments, such as targeted therapy and radiation therapy.
- Targeted therapy. Targeted therapy uses medicines that attack specific chemicals in the cancer cells. By blocking these chemicals, targeted treatments can cause cancer cells to die. Targeted therapy is usually used with chemotherapy.
- Immunotherapy. Immunotherapy is a treatment with medicine that helps the body’s immune system kill cancer cells. The immune system fights off diseases by attacking germs and other cells that shouldn’t be in the body. Cancer cells survive by hiding from the immune system. Immunotherapy helps the immune system cells find and kill the cancer cells.For squamous cell carcinoma of the skin, immunotherapy might be considered when the cancer is advanced and other treatments aren’t an option.
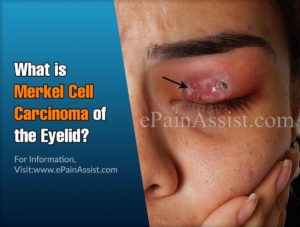
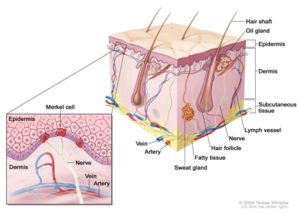
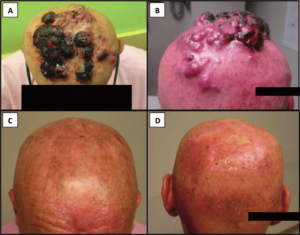
4-Merkel Cell Carcinoma
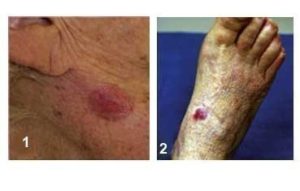
This is a type of skin cancer characterized by flesh-colored nodule that occurs on the face, head or neck. It begins in the cells at the base of the uppermost layer of the skin (epidermis). A normal Merkel cell is a cross between a nerve cell and an endocrine (or hormone-producing) cell located on or just below the skin in the underlying tissue, and functions predominantly as a touch receptor. Merkel cell carcinoma occurs when these cells begin to grow uncontrollably.
Merkel cell tumors typically arise on, but are not limited to, sun-exposed parts of the body such as the face and neck. Their shape and color are less distinctive than other skin cancers, and they can often appear as an innocent pink pearly nodule. As a result, it is usually only the speed with which they grow that attracts the attention of patients and their doctors.
With early detection and treatment, Merkel cell carcinoma can be well contained and even cured. Treatment becomes more difficult as the tumor grows and spreads, but aggressive therapy can still lead to high rates of survival.
Again, Warning Signs can help with early detection and treatment this can be successfully removed without complications. Look out for any new, changing or unusual skin growths, get yourself to the doctor immediately so you can spot skin cancers like BCC when they are easiest to treat and cure.
Risk Factors of Merkel Cell Carcinoma:
–UV exposure from the sun or indoor tanning.
-History of skin cancer, including squamous cell carcinoma (SCC) or melanoma
– Age over 50: Most BCCs appear in people over age 50.
-Fair skin: People with fair skin have an increased risk.
-Male gender: Men are more likely to develop Basal Cell Carcinoma.
-Merkel Cell Virus. Recently, researchers have linked a virus to many cases of Merkel cell carcinoma. However, it remains to be determined if the Merkel cell polyomarvirus causes the disease, and if it might help guide future treatment. If so, the virus could offer promising new targets for immunotherapy.
IT’S A FACT, Memorial Sloan Kettering Hospital in NYC states “Merkel cell carcinoma, also called neuroendocrine cancer of the skin, is an aggressive type of skin cancer that affects only about 400 people in the United States each year. But like other skin cancers, that number is growing.”.
Treatments:
Treatment of stage I and stage II Merkel cell carcinoma:
- Surgery to remove the tumor, such as wide local excision with or without lymph node dissection.
- Radiation therapy after surgery.
Treatment of stage III:
- Wide local excision with or without lymph node dissection.
- Radiation therapy.
- Immunotherapy (immune checkpoint inhibitor therapy using pembrolizumab), for tumors that cannot be removed by surgery.
- A clinical trial of chemotherapy.
- A clinical trial of immunotherapy (nivolumab).
Treatment of Stage IV Merkel Cell Carcinoma
- Immunotherapy (immune checkpoint inhibitor therapy using avelumab or pembrolizumab).
- Chemotherapy, surgery or radiation therapy as palliative treatment to relieve symptoms and improve quality of life.
- A clinical trial of immunotherapy (nivolumab and ipilimumab).