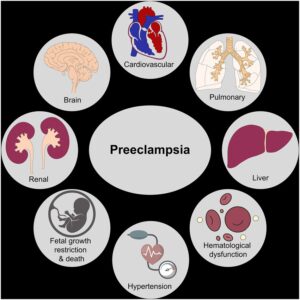
The Box below shows the organs Pre-eclampsia can effect:
What is Preeclampsia?
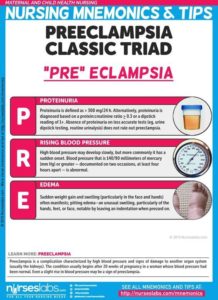
Preeclampsia is a condition that occurs only during pregnancy. Some symptoms may include high blood pressure and protein in the urine, occurring after week 20 of pregnancy. Preeclampsia is often precluded by gestational hypertension. While high blood pressure during pregnancy does not necessarily indicate preeclampsia, it may be a sign of another problem. The condition affects at least 5-8% of pregnancies.
Preeclampsia, formerly called toxemia, is when a pregnant woman has high blood pressure, protein in her urine, and swelling in her legs, feet, and hands. It can range from mild to severe. It usually happens late in pregnancy, though it can come earlier or just after delivery.
Preeclampsia can lead to eclampsia, a serious condition that can have health risks for mom and baby and, in rare cases, cause death. Women with preeclampsia who have seizures have eclampsia.
If you have a mild case and your baby has not reached full development, your doctor will probably recommend you do the following:
- Rest, lying on your left side to take the weight of the baby off your major blood vessels.
- Increase prenatal checkups.
- Consume less salt
- Drink at least 8 glasses of water a day
- Change your diet to include more protein
If you have a severe case, your doctor may try to treat you with blood pressure medication until you are far enough along to deliver safely, along with possibly bed rest, dietary changes, and supplements.
The only cure for preeclampsia is to give birth. Even after delivery, symptoms of preeclampsia can last 1 to 6 weeks or more.
You can help protect yourself by learning the symptoms of preeclampsia and by seeing your doctor for regular prenatal care. Catching preeclampsia early may lower the chances of long-term problems for both mom and baby.
For many years preeclampsia has been considered to be a two-stage disease. The first stage comprises poor placentation. The second stage is the clinical expression of the disease namely new hypertension and new proteinuria in the patient.
Who is at risk for preeclampsia?
- A first-time mom
- Previous experience with gestational hypertension or preeclampsia
- Women whose sisters and mothers who had preeclampsia (family history)
- Women carrying multiple babies
- Women younger than 20 years and older than age 35
- Women who had high blood pressure or kidney disease prior to pregnancy
- Women who are obese or have a BMI of 30 or greater
- Complications in previous pregnancy.
Preeclampsia Causes
Many experts think preeclampsia and eclampsia happen when a woman’s placenta doesn’t work the way it should, but they don’t know exactly why. Some think poor nutrition or high body fat might contribute. A lack of blood flow to the uterus could play a role. Genes are also a factor.
How do I know if I have preeclampsia?
At each prenatal checkup, your healthcare provider will check your blood pressure, urine levels, and may order blood tests which may show if you have preeclampsia. Your physician may also perform other tests that include: checking kidney and blood-clotting functions; ultrasound scan to check your baby’s growth; and Doppler scan to measure the efficiency of blood flow to the placenta.
Symptoms:
Preeclampsia sometimes develops without any symptoms. High blood pressure may develop slowly, or it may have a sudden onset. Monitoring your blood pressure is an important part of prenatal care because the first sign of preeclampsia is commonly a rise in blood pressure. Blood pressure that exceeds 140/90 millimeters of mercury (mm Hg) or greater — documented on two occasions, at least four hours apart — is abnormal.
Other signs and symptoms of preeclampsia may include:
- Excess protein in your urine (proteinuria) or additional signs of kidney problems
- Severe headaches
- Changes in vision, including temporary loss of vision, blurred vision or light sensitivity
- Upper abdominal pain, usually under your ribs on the right side
- Nausea or vomiting
- Decreased urine output
- Decreased levels of platelets in your blood (thrombocytopenia)
- Impaired liver function
- Shortness of breath, caused by fluid in your lungs
When to go to the doctor:
Make sure you attend your prenatal visits so that your health care provider can monitor your blood pressure. Contact your provider immediately or go to an emergency room if you have severe headaches, blurred vision or other visual disturbances, severe belly pain, or severe shortness of breath.
Because headaches, nausea, and aches and pains are common pregnancy complaints, it’s difficult to know when new symptoms are simply part of being pregnant and when they may indicate a serious problem — especially if it’s your first pregnancy. If you’re concerned about your symptoms, contact your doctor.
Complications may include:
- Fetal growth restriction. Preeclampsia affects the arteries carrying blood to the placenta. If the placenta doesn’t get enough blood, the baby may receive inadequate blood and oxygen and fewer nutrients. This can lead to slow growth known as fetal growth restriction.
- Preterm birth. Preeclampsia may lead to an unplanned preterm birth — delivery before 37 weeks. Also, planned preterm birth is a primary treatment for preeclampsia. A baby born prematurely has increased risk of breathing and feeding difficulties, vision or hearing problems, developmental delays, and cerebral palsy. Treatments before preterm delivery may decrease some risks.
- Placental abruption. Preeclampsia increases your risk of placental abruption. With this condition, the placenta separates from the inner wall of the uterus before delivery. Severe abruption can cause heavy bleeding, which can be life-threatening for both the mother and baby.
- hemolysis elevated liver enzymes and low platelet count (HELLP) syndrome. HELLP stands for hemolysis (the destruction of red blood cells), elevated liver enzymes and low platelet count. This severe form of preeclampsia affects several organ systems. HELLP syndrome is life-threatening to the mother and baby, and it may cause lifelong health problems for the mother.Signs and symptoms include nausea and vomiting, headache, upper right belly pain, and a general feeling of illness or being unwell. Sometimes, it develops suddenly, even before high blood pressure is detected. It also may develop without any symptoms.
- Eclampsia. Eclampsia is the onset of seizures or coma with signs or symptoms of preeclampsia. It is very difficult to predict whether a patient with preeclampsia will develop eclampsia. Eclampsia can happen without any previously observed signs or symptoms of preeclampsia.Signs and symptoms that may appear before seizures include severe headaches, vision problems, mental confusion or altered behaviors. But, there are often no symptoms or warning signs. Eclampsia may occur before, during or after delivery.
- Other organ damage. Preeclampsia may result in damage to the kidneys, liver, lung, heart, or eyes, and may cause a stroke or other brain injury. The amount of injury to other organs depends on how severe the preeclampsia is.
- Cardiovascular disease. Having preeclampsia may increase your risk of future heart and blood vessel (cardiovascular) disease. The risk is even greater if you’ve had preeclampsia more than once or you’ve had a preterm delivery.
Prevention of preeclampsia:
Medication
The best clinical evidence for prevention of preeclampsia is the use of low-dose aspirin. Your primary care provider may recommend taking an 81-milligram aspirin tablet daily after 12 weeks of pregnancy if you have one high-risk factor for preeclampsia or more than one moderate-risk factor.
It’s important that you talk with your provider before taking any medications, vitamins or supplements to make sure it’s safe for you.
Lifestyle and healthy choices
Before you become pregnant, especially if you’ve had preeclampsia before, it’s a good idea to be as healthy as you can be. Talk to your provider about managing any conditions that increase the risk of preeclampsia.