What you need to know about sleep:
You’re tired. You could put your head down on a desk right now and fall asleep immediately. You went to bed late last night, had trouble falling asleep and woke up too early. And let’s not kid ourselves: Tonight will be the same unless … well, read on.
This is the classic not-so-shut-eye experience of many Americans who think they are sleep-deprived and possibly need pills or other treatment to fix their insomnia, teeth grinding, jet lag, restless or jerky legs, snoring, sleepwalking and so forth.
Reality is quite different.
For instance, insomnia is said to be the most common sleep disorder, but these dissatisfying sleep experiences only get in the way of daily activities for 10 percent of us, according to the National Institutes of Health. And in almost half of those cases, the real underlying problem is illness (often mental) or the effects of a substance, like coffee or medication.
Here are five recent findings that might help you rest easier:
1. We sleep better than we think we do
For most of us, sleep deprivation is a myth. We’re not zombies. The non-profit National Sleep Foundation (which takes money from the sleep-aid industry, including drug companies that make sleeping pills) says the average U.S. resident gets 7 hours a night and that’s not enough, but a University of Maryland study earlier this year shows we typically get 8 hours and are doing fine. In fact, Americans get just as much sleep nowadays as they did 40 years ago, the study found.
2. We need less sleep as we age
We’ll die without sleep. The details are sketchy, but research suggests it’s a time when we restore vital biological processes and also sort and cement memories. Last year, the World Health Organization determined that nightshift work, which can lead to sleep troubles, is a probable human carcinogen. On the upside, the latest research suggests we need less of it as we get older.
3. You can sleep like a baby (or Thomas Edison)
Multiple, shorter sleep sessions nightly, rather than one long one, are an option. So-called polyphasic sleep is seen in babies, the elderly and other animals (and Thomas Edison reportedly slept this way). For the rest of us, it is more realistic and healthy to sleep at night as best we can and then take naps as needed. EEGs show that we are biphasic sleepers with two alertness dips — one at night time and one mid-day. So talk to HR about setting up a nap room, like they have for NASA’s Phoenix mission team members.
4. Animals exhibit a range of sleep habits
The three-toed sloth sleeps 9.6 hours nightly. But newborn dolphins and killer whales can forgo sleeping for their entire first month. However, the latter extreme is not recommended for humans. We grow irritable and lose our ability to focus and make decisions after even one night of missed sleep, and that can lead to serious accidents driving and using other machinery.
5. Get used to being tired, hit the desk
The bottom line is that a good night’s sleep is within the reach of most of us if we follow common-sense guidelines for sleep hygiene:
- Go to bed at the same time nightly.
- Set aside enough time to hit that golden 7 hours of sleep.
- Refrain from caffeine, heavy or spicy foods, and alcohol and other optional medications that might keep you awake, four to six hours before bed-time.
- Have a pre-sleep routine so you wind down before you hop in.
- Block out distracting lights and noises.
- Only engage in sleep and sex in bed (no TV-watching, reading or eating).
- Exercise regularly but not right before bed.
But you already know all this and you don’t do it. So your realistic plan might be to surrender to the mid-day desk nap.
Exploding Head Syndrome (EHS)
Exploding head syndrome (EHS) is a disorder characterized by the perception of loud noises (e.g. a bomb explosion, gunshot or cymbal crash) when going to sleep or awakening. Contrary to the name, EHS is not associated with pain. However the noise attacks can elicit a great deal of fear, confusion and distress in sufferers. Reports of tachycardia and palpitations are also common. Despite the distressing nature of EHS, relatively little is known about the prevalence and underlying cause of the condition. Some scientists have estimated that EHS may affect 10% of the population. Females tend to be more at risk than males and the average age of onset is 50 years old.
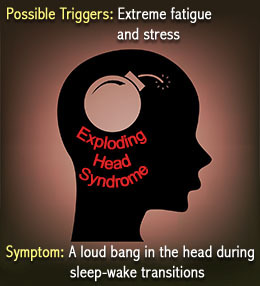
Stress and exploding head syndrome
A few sufferers hear the noise in only one ear, while others hear it in both ears. In other cases, the sound seems to come from inside the patient’s own head (thus the condition’s name).
Most researchers find that exploding head syndrome often occurs in people who are dealing with high levels of stress and physical or mental fatigue. It affects both men and women, though the condition appears more commonly in women, and among people 50 years and older (though it’s also been reported in children).
Because there’s been little research into the condition, nobody is certain what causes exploding head syndrome. Some experts have speculated that it’s related to minor seizures in the brain’s temporal lobe; others suggest it might be related to hearing disorder
Doin’ the hypnagogic jerk
Exploding head syndrome is one of several conditions described as hypnagogic, or occurring in the transitional state between sleep and full wakefulness.
The “hypnagogic jerk” is an involuntary muscle spasm or twitch that occurs as a person is drifting off to sleep.
The muscle spasms may occur spontaneously or may be induced by sound, light or other external stimuli. Some people report hypnagogic jerks accompanied by hallucinations, dreams, the sensation of falling, or bright lights and loud noises coming from inside the head.
As with exploding head syndrome, researchers aren’t sure why hypnogogic jerks occur, but a few theories exist. One hypothesis says that these events are a natural part of the body’s transition from alertness to sleep, and occur when nerves “misfire” during the process.
Another popular idea takes a more evolutionary approach to hypnogogic jerks, explaining that the spasms are an ancient primate reflex responding to the relaxation of muscles at the onset of sleep — the brain misinterprets the relaxation as a sign that the sleeping primate is falling out of a tree, and causes the muscles to quickly react.
Is there a cure for exploding head syndrome?
When exploding head syndrome is related to stress or fatigue, experts recommend stress-management techniques such as yoga, meditation or simply a hot bath before sleeping.
Doctors have reported that many sleep disturbances like exploding head syndrome are related to the use of certain medications or drugs, according to the ASA. Moderating the use of these drugs may alleviate the symptoms of exploding head syndrome.
Some evidence suggests that clomipramine, a member of an older class of tricyclic antidepressants, can help treat exploding head syndrome.
For many patients, the condition comes and goes, disappearing for long stretches at a time, then eventually going away entirely on its own.
There are various theories as to what might cause EHS. For instance, some scientists have speculated that EHS may be associated with minor temporal lobe seizures. Another theory is that EHS is caused by sudden shifts of middle ear components. Other possible causes include stress/anxiety, impairments in calcium signalling and brainstem neuronal dysfunction.
Fortunately, exploding head syndrome is not as dangerous as it sounds.
But it is a real condition, and researchers are finally beginning to seriously investigate the rare and little-understood sleep disorder.
People with exploding head syndrome hear extremely loud noises — a gunshot, an explosion, a thunderclap — as they’re drifting off to sleep, or as they wake up from a deep sleep.
When exploding head syndrome is related to stress or fatigue, experts recommend stress-management techniques such as yoga, meditation or simply a hot bath before sleeping.
Doctors have reported that many sleep disturbances like exploding head syndrome are related to the use of certain medications or drugs, according to the ASA. Moderating the use of these drugs may alleviate the symptoms of exploding head syndrome.
Because of the benign nature of EHS, many individuals do not require medical treatment. However if an individual is suffering from disturbed sleep or considerable distress as a consequence of EHS, then treatment may be necessary. Tricyclic antidepressants have been proven useful in some individuals. Some evidence suggests that clomipramine, a member of an older class of tricyclic antidepressants, can help treat exploding head syndrome. Calcium channel blockers may also be beneficial. Non-pharmacological strategies such as relaxation, improved sleep hygiene and counselling may also help to alleviate symptoms.
For many patients, the condition comes and goes, disappearing for long stretches at a time, then eventually going away entirely on its own.