Learn the S/S Robin Williams had,which where 3 of 4 of these:
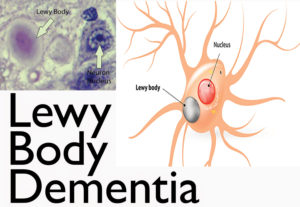
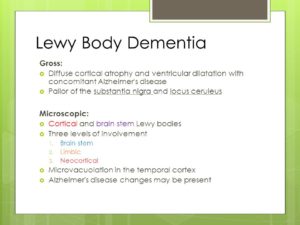
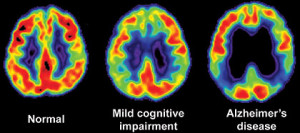
“Who was Lewy? In the early 1900s, while researching Parkinson’s disease, the scientist Friederich H. Lewy discovered abnormal protein deposits that disrupt the brain’s normal functioning. These Lewy body proteins are found in an area of the brain stem where they deplete the neurotransmitter dopamine, causing Parkinsonian symptoms.
In Lewy Body Dementia [LBD], these abnormal proteins are diffuse throughout other areas of the brain, including the cerebral cortex. The brain chemical acetylcholine is depleted, causing disruption of perception, thinking and behavior. Lewy body disease exists either in pure form, or in conjunction with other brain changes, including those typically seen in Alzheimer’s disease and Parkinson’s disease.”
We all know Robin Williams and initially he was presented in the news as committing suicide but in the past few years it has been presented by doctors that he died of LBD which makes more sense, for a man who had it all to many with Parkinson’s Disease. Robin all his life wanted to make others smile and laugh, never did he come across as a depressed unhappy man. We all have our ups and downs along our journey living, which is a part of life. Killing yourself is a severe extreme and you know the news (jump at the first juicy article to make it big or and if we are wrong will admit it or possibly apologize later, sad). The disease killed him in making him think to do suicide.
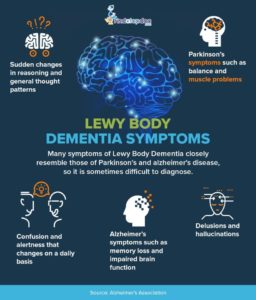
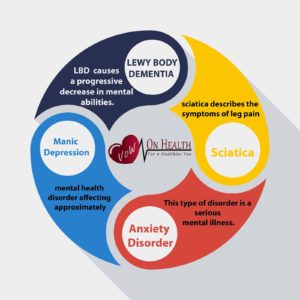
LBD is not a rare disease. It affects an estimated 1.4 million individuals and their families in the United States. Because LBD symptoms can closely resemble other more commonly known diseases like Alzheimer’s and Parkinson’s, it is currently widely underdiagnosed. Many doctors or other medical professionals still are not familiar with LBD.
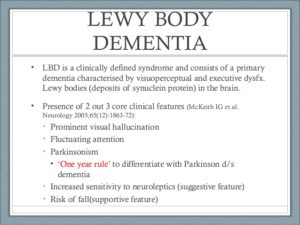
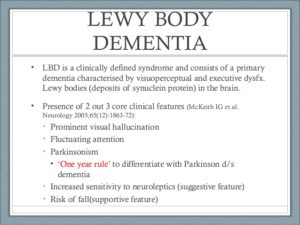
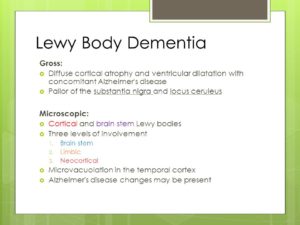
Lewy body dementia (LBD) is a progressive brain disorder in which Lewy bodies (abnormal deposits of a protein called alpha-synuclein) build up in areas of the brain that regulate behavior, cognition, and movement.
A complex disease, LBD can present with a range of symptoms including problems with thinking, memory, moving, sleep and/or changes in behavior, to name a few of the physical, cognitive, and behavioral symptoms.
LBD also affects autonomic body functions, such as blood pressure control, temperature regulation, and bladder and bowel function. Progressively debilitating, LBD can also cause people to experience visual hallucinations or act out their dreams.
What is the Difference Between LBD and Dementia with Lewy Bodies?
LBD is an umbrella term for two closely related clinical diagnoses: Parkinson’s disease dementia and dementia with Lewy bodies (DLB).
What Causes LBD?
The causes of LBD are not yet well understood, but research is ongoing in this area. There are probably multiple factors involved, including genetic and environmental risk factors that combine with natural aging processes to make someone susceptible to LBD.
What are the Signs and Symptoms of LBD?
This condition impairs thinking, such as memory, executive function (planning, processing information), or the ability to understand visual information. Patients with LBD may have fluctuations in attention or alertness; problems with movement including tremors, stiffness, slowness and difficulty walking; hallucinations; and alterations in sleep and behavior.
Come back tomorrow for Part II!