Chronic Obstructive Pulmonary Disease (COPD) is largely preventable. Yet it affects over 15 million Americans and is the fourth leading cause of death in the U.S. Although many diseases have seen a gradual decline in their associated mortality, COPD rates have increased. The term COPD is a broad one used to describe a set of symptoms, referring to persistent, slowly progressive obstruction of airflow and dyspnea, that is predominantly irreversible. It may be caused by chronic bronchitis, emphysema, or bronchiectasis.
People with COPD experience deterioration in functional status; therefore, improving function is a major goal of treatment. Nurses are often facilitators and coordinators of pulmonary rehabilitation. Evaluation of the effects of treatment is an essential aspect of providing quality care. Although some effects of COPD are permanent, you can do plenty to assist your patient in managing it, by educating him on how to gain back control of his health. This will help to decrease the depression, hopelessness, and pessimism that are commonly seen in patients with COPD.
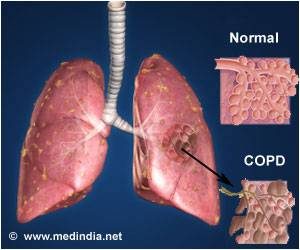
Chronic obstructive pulmonary disease (COPD) is a term that applies to patients with chronic bronchitis, bronchiectasis, emphysema and, to a certain extent, asthma. A brief review of normal functional anatomy will provide a background for the discussion of pathology.
The airway down to the bronchioles normally is lined with ciliated pseudo-stratified columnar cells and goblet cells. Mucus derives from mucus glands that are freely distributed in the walls of the trachea and bronchi. The cilia sweep mucus and minor debris toward the upper airway. Low humidity, anesthesia gases, cigarette smoking and other chemical irritants paralyze the action of these cilia. The mucociliary action starts again after a matter of time. This is why people awaken to “smokers cough.”
“Chronic obstructive pulmonary disease (COPD) is a term that applies to patients with chronic bronchitis, bronchiectasis, emphysema and, to a certain extent, asthma.”
Bronchi run in septal connective tissue, but bronchioles are suspended in lung parenchyma by alveolar elastic tissue. The elastic tissue extends throughout alveolar walls, air passages, and vessels, connecting them in a delicate web. Bronchiolar epithelium is ciliated, single-layered and columnar or cuboidal. Beyond the bronchioles the epithelium is flat and lined with a film of phospholipid (surfactant), which lowers surface tension and thereby helps to keep these air spaces from collapsing. Remember that the phospholipid develops during later gestation in utero. This is the reason why premature infant’s lungs cannot stay inflated without the addition of surfactant therapy. Macrophages are found in alveolar lining. Smooth muscles surround the walls of all bronchi, bronchioles, and alveolar ducts and when stimulated they shorten and narrow the passages. Cartilage lends rigidity and lies in regular horse-shaped rings in the tracheal wall. Cartilage is absent in bronchi less than 1 mm in diameter.
The terminal bronchiole is lined with columnar epithelium and is the last purely conducting airway. An acinus includes a terminal bronchiole and its distal structures. Five to ten acini together constitute a secondary lobule, which is generally 1 to 2 cm in diameter and is partly surrounded by grossly visible fibrous septa. Passages distal to the terminal bronchiole include an average of three but as many as nine generations of respiratory bronchioles lined with both columnar and alveolar epithelium. Each of the last respiratory bronchioles gives rise to about six alveolar ducts, each of these to one or two alveolar sacs, and finally each of the sacs to perhaps seventy-five alveoli. Alveolar pores (pores of Kohn) may connect alveoli in adjacent lobules.
Two different circulations supply the lungs. The pulmonary arteries and veins are involved in gas exchange. The pulmonary arteries branch with the bronchi, dividing into capillaries at the level of the respiratory bronchiole, and supplying these as well as the alveolar ducts and alveoli. In the periphery of the lung, the pulmonary veins lie in the interlobular septa rather than accompanying the arteries and airways. The bronchial arteries are small and arise mostly from the aorta. They accompany the bronchi to supply their walls. In some cases of COPD, like bronchiectasis, extensive anastomoses develop between the pulmonary and bronchial circulations. This can allow major shunting and recirculation of blood, therefore contributing to cardiac overload and failure. Lymphatics run chiefly in bronchial walls and as a fine network in the pleural membrane. The lumina of the capillaries in the alveolar walls are separated from the alveolar lining surfaces by the alveolar-capillary membrane, consisting of thin endothelial and epithelial cells and a minute but expansile interstitial space. This interface between air and blood, only 2 microns in thickness, is the only place where gases may be exchanged effectively.
Disease Specific Review
Chronic Bronchitis
Chronic bronchitis is a clinical disorder characterized by excessive mucus secretion in the bronchi. It was traditionally defined by chronic or recurrent productive cough lasting for a minimum of three months per year and for at least two consecutive years, in which all other causes for the cough have been eliminated. Today’s definition remains more simplistic to include a productive cough progressing over a period of time and lasting longer and longer. Sometimes, chronic bronchitis is broken down into three types: simple, mucopurulent or obstructive. The pathologic changes consist of inflammation, primarily mononuclear, infiltrate in the bronchial wall, hypertrophy and hyperplasia of the mucus-secreting bronchial glands and mucosal goblet cells, metaplasia of bronchial and bronchiolar epithelium, and loss of cilia. Eventually, there may be distortion and scarring of the bronchial wall.
Asthma
Asthma is a disease characterized by increased responsiveness of the trachea and bronchi to various stimuli (intrinsic or extrinsic), causing difficulty in breathing due to narrowing airways. The narrowing is dynamic and changes in degree. It occurs either spontaneously or because of therapy. The basic defect appears to be an altered state of the host, which periodically produces a hyperirritable contraction of smooth muscle and hypersecretion of bronchial mucus. This mucus is abnormally sticky and therefore obstructive. In some instances, the illness seems related to an altered immunologic state.
Histological changes of asthma include an increase in the size and number of the mucosal goblet cells and submucosal mucus glands. There is marked thickening of the bronchial basement membrane and hypertrophy of bronchial and bronchiolar smooth muscle tissue. A submucosal infiltration of mononuclear inflammatory cells, eosinophils and plugs of mucus blocks small airways. Patients who have had asthma for many years may develop cor pulmonale and emphysema.
Emphysema
Pulmonary emphysema is described in clinical, radiological and physiologic terms, but the condition is best defined morphologically. It is an enlargement of the air spaces distal to the terminal non-respiratory bronchiole, with destruction of alveolar walls.
Although the normal lung has about 35,000 terminal bronchioles and their total internal cross-sectional area is at least 40 times as great as that of the lobar bronchi, the bronchioles are more delicate and vulnerable. Bronchioles may be obstructed partially or completely, temporarily or permanently, by thickening of their walls, by collapse due to loss of elasticity of the surrounding parenchyma, or by influx of exudate. In advanced emphysema, the lungs are large, pale, and relatively bloodless. They do not readily collapse. They many contain many superficial blebs or bullae, which occasionally are huge. The right ventricle of the heart is often enlarged (cor pulmonale), reflecting pulmonary arterial hypertension. Right ventricular enlargement is found in about 40% of autopsies of patients with severe emphysema. The distal air spaces are distended and disrupted, thus excessively confluent and reduced in number. There may be marked decrease in the number and size of the smaller vascular channels. The decrease in alveolar-capillary membrane surface area may be critical. Death may result from infection that obliterates the small bronchi and bronchioles. There is often organized pneumonia or scarring of the lung parenchyma due to previous infections.
Classification of emphysema relies on descriptive morphology, requiring the study of inflated lungs. The two principal types are centrilobular and panlobular emphysema. The two types may coexist in the same lung or lobe.
Centrilobular emphysema (CLE) or centriacinar emphysema affects respiratory bronchioles selectively. Fenestrations develop in the walls, enlarge, become confluent, and tend to form a single space as the walls disintegrate. There is often bronchiolitis with narrowing of lumina. The more distal parenchyma (alveolar ducts and sacs and alveoli) is initially preserved, then similarly destroyed as fenestrations develop and progress.
The disease commonly affects the upper portions of the lung more severely, but it tends to be unevenly distributed. The walls of the emphysematous spaces may be deeply pigmented. This discoloration may represent failure of clearance mechanisms to remove dust particles, or perhaps the pigment plays an active role in lung destruction. CLE is much more prevalent in males than in females. It is usually associated with chronic bronchitis and is seldom found in nonsmokers.
Panlobular emphysema (PLE) or panacinar emphysema is a nearly uniform enlargement and destruction of the alveoli in the pulmonary acinus. As the disease progresses, there is gradual loss of all components of the acinus until only a few strands of tissue, which are usually blood vessels, remain. PLE is usually diffuse, but is more severe in the lower lung areas. It is often found to some degree in older people, who do not have chronic bronchitis or clinical impairment of lung function. The term senile emphysema was formerly applied to this condition. PLE occurs as commonly in women and men, but is less frequent than CLE. It is a characteristic finding in those with homozygous deficiency of serum alpha-1 antitrypsin. It has also been found that certain populations of IV Ritalin abusers show PLE.
Bullae are common in both CLE and PLE, but may exist in the absence of either. Air-filled spaces in the visceral pleura are commonly termed blebs, and those in the parenchyma greater than 1 cm in diameter are called bullae. A valve mechanism in the bronchial communication of a bulla permits air trapping and enlargement of the air space. This scenario may compress the surrounding normal lung. Blebs may rupture into the pleural cavity causing a pneumothorax, and through a valve mechanism in the bronchopleural fistula a tension pneumothorax may develop.
Paracicatricial emphysema occurring adjacent to pulmonary scars represents another type of localized emphysema. When the air spaces distal to terminal bronchioles are increased beyond the normal size but do not show destructive changes of the alveolar walls, the condition is called pulmonary overinflation. This condition may be obstructive, because of air trapping beyond an incomplete bronchial obstruction due to a foreign body or a neoplasm. Many lung lobules may be simultaneously affected as a result of many check-valve obstructions, as in bronchial asthma. Pulmonary overinflation may also be nonobstructive, less properly called “compensatory emphysema”, when associated with atelectasis or resection of other areas of the lung.
Bronchiectasis
Bronchiectasis means irreversible dilation and distortion of the bronchi and bronchioles. Saccular bronchiectasis is the classic advanced form characterized by irregular dilatations and narrowing. The term cystic is used when the dilatations are especially large and numerous. Cystic bronchiectasis can be further classified as fusiform or varicose.
Tubular bronchiectasis is simply the absence of normal bronchial tapering and is usually a manifestation of severe chronic bronchitis rather than of true bronchial wall destruction.
Repeated or prolonged episodes of pneumonitis, inhaled foreign objects or neoplasms have been known to cause bronchiectasis. When the bronchiectatic process involves most or all of the bronchial tree, whether in one or both lungs, it is believed to be genetic or developmental in origin.
Mucoviscidosis, Kartagener’s syndrome (bronchiectasis with dextrocardia and paranasal sinusitis), and agammaglobulinemia are all examples of inherited or developmental diseases associated with bronchiectasis. The term pseudobronchiectasis is applied to cylindrical bronchial widening, which may complicate a pneumonitis but which disappears after a few months. Bronchiectasis is true saccular bronchiectasis but without cough or expectoration. It is located especially in the upper lobes where good dependent drainage is available. A proximal form of bronchiectasis (with normal distal airways) complicates aspergillus mucus plugging.
Advanced bronchiectasis is often accompanied by anastomoses between the bronchial and pulmonary vessels. These cause right-to-left shunts, with resulting hypoxemia, pulmonary hypertension and cor pulmonale.
Etiology & Pathogenesis
Etiology
By far the most common etiological cause of COPD remains smoking. Even after the client quits smoking, the disease process continues to worsen. Air pollution and occupation also play an important role in COPD. Smog and second-hand smoke contribute to worsening of the disease.
Occupational exposure to irritating fumes and dusts may aggravate COPD. Silicosis and other pneumonoconioses may bring about lung fibrosis and focal emphysema. Exposure to certain vegetable dusts, such as cotton fiber, molds and fungi in grain dust, may increase airway resistance and sometimes produce permanent respiratory impairment. Exposures to irritating gases, such as chlorine and oxides of nitrogen and sulfur, produce pulmonary edema, bronchiolitis and at times permanent parenchymal damage.
Repeated bronchopulmonary infections can also intensify the existing pathological changes, playing a role in destruction of lung parenchyma and the progression of COPD.
Heredity or biological factors can determine the reactions of pulmonary tissue to noxious agents. For example, a genetic familial form of emphysema involves a deficiency of the major normal serum alpha-1 globulin (alpha-1 antitrypsin). A single autosomal recessive gene transmits this deficiency. The homozygotes may develop severe panlobular emphysema (PLE) early in adult life. The heterozygotes appear to be predisposed to the development of centrilobular emphysema related to cigarette smoking. The other better-known cause of chronic lung disease is mucoviscidosis or cystic fibrosis, which produces thickened secretions via the endocrine system and throughout the body.
Aging by itself is not a primary cause of COPD, but some degree of panlobular emphysema is commonly discovered on histopathologic examination. Age related dorsal kyphosis with the barrel-shaped thorax has often been called senile emphysema, even though there is little destruction of interalveolar septa. The morphologic changes consist of dilated air spaces and pores of Kohn.
Pathogenesis
The pathogenesis of COPD is not fully understood despite attempts to correlate the morphologic appearance of lungs at necropsy to the clinical measurements of functioning during life. Chronic bronchitis and centrilobular emphysema do seem to develop after prolonged exposure to cigarette smoke and/or other air pollutants. Whatever the causes, bronchiolar obstruction by itself does not result in focal atelectasis, provided there is collateral ventilation from adjacent pulmonary parenchyma via the pores of Kohn.
It has been proposed that airway obstruction at times may result in a check-valve mechanism leading to overdistension and rupture of alveolar septa, especially if the latter are inflamed and exposed to high positive pressure (i.e. barotrauma). This concept of pathogenesis of emphysema is entirely speculative. Airflow obstruction alone does not necessarily result in tissue destruction. Moreover, both centrilobular and panlobular emphysema may exist in lungs of asymptomatic individuals. It has been reported that up to 30% of lung tissue can be destroyed by emphysema without resulting in demonstrable airflow obstruction. Normally, radial traction forces of the attached alveolar septa support the bronchiolar walls. With loss of alveolar surface in emphysema, there is a decrease in surface tension, resulting in expiratory airway collapse. Additional investigative work continues in an effort to link disease states to pathogenesis.
Treatment of COPD
By far the best ways to treat COPD are to catch it early and to stop smoking. The physician-client relationship requires realistic expectations to keep the client from becoming too depressed or discouraged. The aim of treatment is to improve or at least to preserve existing lung function and to help the client to adapt to the limitations imposed by his illness. The physician needs to let the client know the signs of acute infection or respiratory distress. Pulse oximetry allows the physician to monitor hypoxia noninvasively.
The nurse-client relationship develops as well, with the nurse often the liaison between the physician and the client. In early stages, cardiopulmonary rehabilitation is of utmost importance to help the client to understand how to pace himself, control his diet/weight, control climate and avoid irritants. It also helps clients learn about medications (including steroid therapy), breathing exercises, and oxygen therapy. The nurse should teach the client to be aware of symptoms of bronchial infections; treatment of cough and sputum retention; how to recognize cor pulmonale and congestive heart failure; and how to recognize a spontaneous pneumothorax, peptic ulcers, arteriosclerotic and hypertensive heart disease, and pulmonary thromboembolic disease. The psychological and economic problems of COPD patients call for sympathy as well as wisdom. Suggestions for retirement or sedentary work often cause resentment. Many times the impairment of mental acuity and judgment force the work issue. The patient needs to learn new habits in walking and pacing his activities. Mild sedation may be needed to keep the dyspneic patient from getting more anxious.
Frequent small meals are recommended. Eating usually results in dyspnea and the resultant air hunger and chewing difficulties can exhaust the COPDer. Mental depression may cause anorexia; sometimes drugs such as theophylline or digitalis may be the offender. The recommended low salt diet to reduce edema can make food less palatable. A 3 to 4 g Na restriction is recommended. Serum zinc tends to run low in many COPDers. Protein is the single, most important nutrient for COPDers on steroids, as they break down more protein than was previously thought.
Healthy individuals consume 36 to 72 calories per day in the energy expenditure of breathing. COPD patients consume an estimated 430 to 720 calories per day, a tenfold increase. They require an average of about 500 calories per day more than people without COPD do. Somewhere between 25 to 65% of COPD patients are plagued with significant weight loss.
It should also be noted that moving to a warm dry climate is usually of no benefit. It is better to live at sea level because at higher elevations there is reduced oxygen tension. Sensitization to allergens seems to work better in younger patients. Of course, inhaled irritants should be avoided; for example, smoking, fumes, extreme cold or hot air, industrial dusts, etc.
Typical drug treatment may Include a variety of medications.
Inhaled corticosteroids may be used to Inflammation In the airways. Examples are beclomethasone (Beclovent, Vanceril), budesonide (Pulmicort), circlesonide (Alvesco), mometesone (Asmanex) and triamcinolone (Azmacort).
In asthma-allergy related bronchospasm, Leukotriene Modifiers may be used. Leukotrienes are natural chemicals that promote bronchoconstriction, mucus production, airway edema and eosinophil Infiltration. There modifiers prevent asthma by blocking these receptors. Examples are Montekukast (Singular), Zafirkulast (Accolate): I.e. use caution when patients also on Theophylline or Warfarin, and Zileuton (Zyflo).
Mast Cell Stabilizers may also be used to decrease the release of histamine. Remember, mast cells release histamine and cause constriction of bronchioles, dilated blood vessels, produces mucus and Increases capillary permeability. Examples are cromolyn (Intal) MDI and nedocromil sodium (Tilade) MDI.
Mucolytics are used to thin mucus. It does so by breaking the disulfide bond In sputum. Example medication Is acetylcysteine (Mucomyst).
Antihistamines may also be needed. They occupy the histamine receptors. There are two types: H1 and H2 receptors.
Commonly used drugs are:
Cetirizine (Zyrtec), Dimenhydrinate (Dramamine), Diphenhydramine hypochloride (Benadryl), Fexofenadine (Allegra), Loratadine (Claritan) and Promethazine (Phenergan).
The most common Intranasal corticosteroids are Beclomethasone (Beconase AQ), Budesonide (Rhinocort), Ciclesonide (Omnaris), flunisolide (Nasalide), fluticasone (Flonase, Veramyst), mometasone (Nasonex) and triamcinolone (Nasocort AQ).
For those suffering from Alpha-1-Antitrypsin deficiency, alpha 1 proteinase Inhibitors may help. Examples are alpha-1-antitrypsin, Aralast, Prolastin and Zemaira.
The most commonly used drugs for COPD are the bronchodilators that relax smooth muscles In the bronchi and bronchioles. There are three major types: adrenergics, xanthines and anticholinergics. Each will be covered.
First, we will discuss the Adrenergics. They act on the beta 2 adrenergic receptors In the smooth muscle of the bronchi and bronchioles. They stimulate Increased production of cyclic adenosine monophosphate (cAMP), which Induces relaxation of the smooth muscle and allows the airways to dilate.
Some adrenergics act on beta 1 adrenergic receptors as well, which results In cardiac stimulation.
Some examples of beta-adrenergics are Albuterol (Proventil, Ventolin, VoSpire), Arformoterol (Brovana), Fomoterol (Foradil, Performist), Levalbuterol (Xopenex), Pirbuterol (Maxair), Salmeterol (Serevent) and Terbutaline (Brethine).
Secondly are the Xanthines. They Increase cAMP, but by a different mechanism. Xanthines Inhibit the enzyme that normally breaks down cAMP. It may cause mild diuresis by Increasing blood flow to the kidneys.
Examples are aminophylline (Truphylline) and theophylline (Theo-dur).
Lastly are the anticholinergics. Given by Inhalation they reduce Intracellular cyclic guanosine (cGMP), a substance that blocks the action of acytlcholine In bronchial smooth muscle.
Examples are Ipratropium (Atrovent, Combivent) and tiotropium (Spiriva). There Is a respiratory mist Inhaler form of Spiriva that has been tested In Europe but Is NOT approved In the U.S. and 55 other countries becausee It has been found to cause one In every 124 patients to die annually compared to the placebo. The handihaler capsules are the safest form of this medication.
Today, between 80-90% of COPD can be blamed on smoking and smoking cessation remains the most effective way to prevent lung damage caused by COPD. Physicians now have more pharmacologic options to treat nicotine addiction, such as Zyban and Wellbutrin. There are contraindications to these drugs so the patient needs to be screened carefully. The latest national guidelines did show improved outcomes.
Up to 70% of terminally ill patients experience dyspnea. Morphine nebulization has proven to be safe in treating dyspnea associated with end-stage COPD, CHF and lung cancer. Its effectiveness is believed to be caused by opioid receptors in the lungs and loosening of secretions. Nebulization is not recommended as a route for analgesia, primarily because current administrative technologies result in very small amounts of analgesic being absorbed. Nebulized morphine has a viable bioavailability of 9-35%.
Other new inhalation medications include Tobramycin [TOBI] an aminoglycoside antibiotic. This aerosolized antibiotic is frequently used in cystic fibrosis patients and requires a specialized nebulizer to insure proper particle size. Side effects are voice alteration and tinnitis. All aminoglycosides have potential to cause tubular necrosis, renal failure, deafness due to cochlear toxicity, vertigo due to damage to vestibular organs and rarely neuromuscular blockade. That is why monitoring peak and trough Tobramycin blood levels are so important.
Many of the newer drugs for asthma are classed as mediators of leukotrienes C4, D4, and E4. They are found to inhibit the process of binding to the specific receptor sites. Zafirlukast [Accolate] uses this mechanism. Other leukotriene modifiers are montelukast [Singular]. Secondly, they found they could use leukotrienes to antagonize the receptor site by interfering with the binding of arachidonic acid to 5-lipoxygenase (5-LO). The drug zileuton [Zyflo] uses this method.
Leukotriene modifiers have received some bad media attention for their association with Churg Strauss Syndrome, a condition presenting flu-like symptoms; fever and muscular aches. Patients develop a vasculitis rash. Progressive pulmonary complications ensue resulting in cardiac failure and labs show increased eosinophils.
Leukotriene modifiers can cause increase in metabolism and excretion of the drug Warfarin, resulting in an increased prothrombin time. Theophylline causes a decrease in the plasma level of Accolate,while aspirin increases the plasma level of this medication.
Zyflo can double the patient’s serum theophylline level but has no reported interaction with aspirin.
By far, in exercised induced asthma sufferer’s, leukotriene modifiers benefits definitely outweigh the risks!
Different types of medications treat different aspects and symptoms of COPD. Your doctor will prescribe medications that will best treat your particular condition.