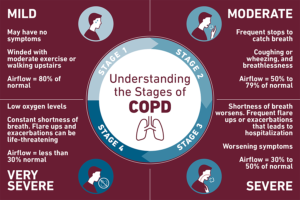
If you have COPD, you may have symptoms such as:
- trouble breathing
- cough
- wheezing
- tightness in your chest
Smoking often causes COPD, but in some cases, breathing in toxins from the environment is the cause.
There’s currently no cure for COPD, and the damage to the lungs and airways is permanent.
However, several medications can help reduce inflammation and open your airways to help you breathe easier with COPD.
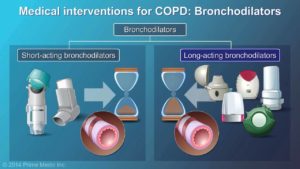
Short Acting Bronchodilators:
Bronchodilators help open your airways to make breathing easier. Your doctor may prescribe short-acting bronchodilators for an emergency situation or for quick relief as needed.
You take them using an inhaler or nebulizer.
Examples of short-acting bronchodilators include:
- albuterol (Proair HFA, Ventolin HFA)
- levalbuterol (Xopenex)
- ipratropium (Atrovent HFA)
- albuterol/ipratropium (Combivent Respimat)
Short-acting bronchodilators can cause side effects such as:
- dry mouth
- headache
- cough
These effects should go away over time.
Other side effects include:
- tremors (shaking)
- nervousness
- a fast heartbeat
If you have a heart condition, tell your doctor before taking a short-acting bronchodilator.
Corticosteroids:
With COPD, your airways can be inflamed, causing them to become swollen and irritated. Inflammation makes it harder to breathe.
Corticosteroids are a type of medication that reduces inflammation in the body, making air flow easier in the lungs.
Several types of corticosteroids are available. Some are inhalable and should be used every day as directed. They’re usually prescribed in combination with a long-acting COPD drug.
Other corticosteroids are injected or taken by mouth. These forms are used on a short-term basis when your COPD suddenly gets worse.
The corticosteroids that doctors most often prescribe for COPD are:
- Fluticasone (Flovent). This comes as an inhaler you use twice daily. Side effects can include headache, sore throat, voice changes, nausea, cold-like symptoms, and thrush.
- Budesonide (Pulmicort). This comes as a handheld inhaler or for use in a nebulizer. Side effects can include colds and thrush.
- Prednisolone. This comes as a pill, liquid, or shot. It’s usually given for emergency rescue treatment. Side effects can include headache, muscle weakness, upset stomach, and weight gain.
Methylxanthines:
For some people with severe COPD, the typical first-line treatments, such as fast-acting bronchodilators and corticosteroids, don’t seem to help when used on their own.
When this happens, some doctors prescribe a drug called theophylline along with a bronchodilator.
Theophylline works as an anti-inflammatory drug and relaxes the muscles in the airways. It comes as a pill or liquid you take daily.
Side effects of theophylline can include:
- nausea or vomiting
- tremors
- headache
- trouble sleeping
Long Acting Bronchodilators:
Long-acting bronchodilators are medications that are used to treat COPD over a longer period of time. They’re usually taken once or twice daily using inhalers or nebulizers.
Because these drugs work gradually to help ease breathing, they don’t act as quickly as rescue medication. They’re not meant to be used in an emergency situation.
The long-acting bronchodilators currently available are:
- aclidinium (Tudorza)
- arformoterol (Brovana)
- formoterol (Foradil, Perforomist)
- glycopyrrolate (Seebri Neohaler, Lonhala Magnair)
- indacaterol (Arcapta)
- olodaterol (Striverdi Respimat)
- revefenacin (Yupelri)
- salmeterol (Serevent)
- tiotropium (Spiriva)
- umeclidinium (Incruse Ellipta)
Side effects of long-acting bronchodilators can include:
- dry mouth
- dizziness
- tremors
- runny nose
- irritated or scratchy throat
- upset stomach
More serious side effects include:
- blurry vision
- rapid or irregular heart rate
- an allergic reaction with rash or swelling
Combination Drugs:
Several COPD drugs come as combination medications. These are mainly combinations of either two long-acting bronchodilators or an inhaled corticosteroid and a long-acting bronchodilator.
For people with COPD who experience shortness of breath or trouble breathing during exercise, the American Thoracic Society strongly recommends a long-acting beta agonist (LABA) combined with a long- acting muscarinic antagonist (LAMA).
Triple therapy, a combination of an inhaled corticosteroid and two long-acting bronchodilators, is recommended for those who continue to have shortness of breath or trouble breathing and are currently using LABA and LAMA combination therapy.
Recommended LABA/LAMA combination bronchodilator therapies include:
- aclidinium/formoterol (Duaklir)
- glycopyrrolate/formoterol (Bevespi Aerosphere)
- tiotropium/olodaterol (Stiolto Respimat)
- umeclidinium/vilanterol (Anoro Ellipta)
Combinations of an inhaled corticosteroid and a long-acting bronchodilator include:
- budesonide/formoterol (Symbicort)
- fluticasone/salmeterol (Advair)
- fluticasone/vilanterol (Breo Ellipta)
Combinations of an inhaled corticosteroid and two long-acting bronchodilators, called triple therapy, include fluticasone/vilanterol/umeclidinium (Trelegy Ellipta).
A 2018 research reviewTrusted Source found that triple therapy reduced flare-ups and improved lung function in people with advanced COPD.
According to current guidelines, the inhaled corticosteroid may be withdrawn if you have not had a flare-up in the past year.
However, it also indicated that pneumonia was more likely to develop with triple therapy than with a combination of two medications.
Antibiotics:
Regular treatment with antibiotics like azithromycin and erythromycin may help manage COPD.
Long term antibiotic therapy needs further research studies.
Cancer Medications for COPD:
Several cancer drugs could possibly help reduce inflammation and limit damage from COPD.
A 2019 study found that the drug tyrphostin AG825 helped lower inflammation levels in zebrafish.
The medication also sped up the rate of death of neutrophils, which are cells that promote inflammation, in mice with inflamed lungs similar to COPD.
Research is still limited on using tyrphostin AG825 and similar drugs for COPD and other inflammatory conditions. Eventually, they may become a treatment option for COPD.
Different types of medications treat different aspects and symptoms of COPD. Your doctor will prescribe medications that will best treat your particular condition.
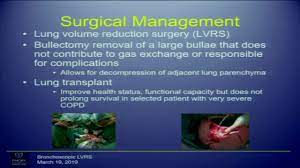
Types of surgery for COPD:
Some considerations for surgery candidates include:
- You must be strong enough to have the surgery.
- You must participate in a pulmonary rehabilitation program.
- You cannot be a current smoker.
Some lung surgeries require that the lung damage must be in an area that is localized (a specific area) and can be removed. The decision for surgery is based on the results of many tests. Talk to your doctor to find out if lung surgery is right for you.
There are two types of lung surgery performed to address COPD:
- Bullectomy is a procedure where doctors remove one or more of the very large bullae or blebs from the lungs. Bullae are large air sacs that form from hundreds of destroyed alveoli. These air spaces can become so large that they crowd out the better functioning lung and interfere with breathing. For those people, removing the destroyed air sacs improves breathing.
- Lung Volume Reduction Surgery (LVRS) is a procedure to help people with severe emphysema affecting the upper lung lobes. LVRS is not a cure for COPD but can improve one’s exercise capacity and quality of life. The goal of the surgery is to reduce the size of the lungs by removing about 30 percent of the most diseased lung tissues so that the remaining healthier portion can perform better. LVRS also can allow the diaphragm to return to its normal shape, helping you breathe more efficiently. The surgery has been shown to help improve breathing ability, lung capacity and overall quality of life among those who qualify for it.
Surgery Transplantation for patients who are candidates:
Lung transplantation can prolong and dramatically improve quality of life for patients with advanced lung diseases. The Center for Advanced Lung Disease and Lung Transplantation at NewYork-Presbyterian/Columbia University Irving Medical Center is one of the oldest in the United States, having performed more than 1,300 lung and heart-lung transplants since 1988. Between 2001 and 2019, with the launch of new program leadership, they performed over 1,000 lung transplants.
Their patient survival rates are much higher than the national average — even though they treat sicker patients than most U.S. centers. We’ve also worked to expand the pool of donor lungs through innovative technologies. Over the years, they have earned a reputation for our clinical expertise and rigorous commitment to excellence.