MSM “Men who have sex with men”
The term “men who have sex with men” (MSM) describes a heterogeneous group of men who have varied behaviors, identities, and health-care needs. Some MSM are at high risk for HIV infection and other viral and bacterial STDs because MSM may practice anal sex, and the rectal mucosa is uniquely susceptible to certain STD pathogens. In addition, multiple sex partners, substance use, and sexual network dynamics of MSM increase risk for HIV and STDs in this population. The frequency of unsafe sexual practices and the reported rates of bacterial STDs and incident HIV infection declined substantially in MSM from the 1980s through the mid-1990s. However, since that time, increased rates of early syphilis (primary, secondary, or early latent), gonorrhea, and chlamydial infection and higher rates of sexual risk behaviors have been documented among MSM in the United States and virtually all industrialized countries.
Approximately two thirds of the cases of primary and secondary syphilis diagnoses in the United States are in MSM, particularly those in ethnic minority groups. Increased syphilis screening in MSM demonstrated a doubling of early syphilis detection; however, 71% of the syphilis diagnoses occurred when the patient sought care for symptoms . Acute HIV infection has been associated with a recent or concurrent STD, including syphilis, among men at a municipal STD clinic. Factors associated with increases in syphilis among MSM have included substance abuse (e.g., methamphetamine), having multiple anonymous partners, and seeking sex partners through the internet.
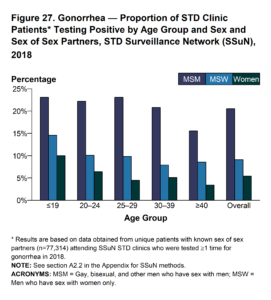
Gonococcal infection in MSM has been associated with similar risk factors, including having multiple anonymous partners and abuse of substances, particularly crystal methamphetamine. Rectal gonococcal rates are increasing among MSM with HIV infection, underscoring the importance of obtaining an accurate, current sexual history and asking about correlates of increased risk (e.g., anonymous sex and substance use). Insertive oral sex has been associated with urethral gonorrhea acquisition.
MSM remain at disproportionate risk for HIV acquisition and transmission in the United States, particularly those who are black or Hispanic. Factors that increase the risk for HIV infection in MSM include either receptive or insertive anal sex without a condom, having another STD, having sex with anonymous partners without a condom, and using methamphetamines or drugs that enhance sexual performance.
Clinicians should routinely ask sexually active MSM about symptoms consistent with common STDs, including urethral discharge, dysuria, genital and perianal ulcers, regional lymphadenopathy, skin rash, and anorectal symptoms consistent with proctitis (e.g., discharge and pain on defecation or during anal intercourse) and then perform appropriate diagnostic testing. In addition, providers should offer evidence-based counseling on safer sex using interventions that have been demonstrated to decrease STD incidence in clinical-care settings.
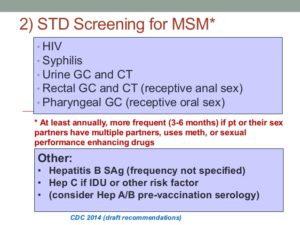
The following screening tests should be performed at least annually for sexually active MSM, including those with HIV infection.
- HIV serology, if HIV status is unknown or negative and the patient himself or his sex partner(s) has had more than one sex partner since most recent HIV test.
- Syphilis serology to establish whether persons with reactive tests have untreated syphilis, have partially treated syphilis, are manifesting a slow serologic response to appropriate prior therapy, or are serofast.
- A test for urethral infection† with N. gonorrhoeae and C. trachomatis in men who have had insertive intercourse§ during the preceding year (testing of the urine using NAAT† is the preferred approach).
- A test for rectal infection† with N. gonorrhoeae and C. trachomatis in men who have had receptive anal intercourse§ during the preceding year (NAAT of a rectal specimen is the preferred approach).
- A test for pharyngeal infection† with N. gonorrhoeae in men who have had receptive oral intercourse§ during the preceding year (NAAT of a pharyngeal specimen is the preferred approach). Testing for C. trachomatis pharyngeal infection is not recommended.
MSM with HIV infection are also at risk for STDs. Data from a study of 557 adults with HIV infection receiving primary care in four U.S. cities demonstrate that 13% had STD at study enrollment, and 7% had incident STD at 6 months; among MSM with HIV infection, STD incidence was 20%. Excluding trichomoniasis, 94% of incident STDs were diagnosed in MSM. All MSM with HIV infection entering care should be screened for gonorrhea and chlamydia at appropriate anatomic sites of exposure, as well as for syphilis. The frequency of follow-up testing might be dictated by subsequent behavior; screening is recommended annually, at a minimum, to include syphilis serologic testing and chlamydia and gonorrhea screening at exposed anatomic sites). STD screening rates in HIV clinics have been suboptimal. In one study involving eight U.S. cities, although syphilis testing was provided to most MSM with HIV infection, <10% were screened for extra-genitourinary gonorrhea or chlamydia, and <20% provided the urine or urethral specimens needed for testing. More frequent STD screening (i.e., for syphilis, gonorrhea, and chlamydia) at 3–6-month intervals is indicated for MSM, including those with HIV infection if risk behaviors persist or if they or their sexual partners have multiple partners. Evaluation for HSV-2 infection with type-specific serologic tests also can be considered if infection status is unknown in persons with previously undiagnosed genital tract infection.
HPV infection and HPV-associated conditions (e.g., anogenital warts and anal squamous intraepithelial lesions) are highly prevalent among MSM. The quadrivalent vaccine is recommended routinely for MSM through age 26 years; the efficacy of this vaccine in preventing HPV associated diseases in men aged >26 years is unknown.
Data are insufficient to recommend routine anal-cancer screening with anal cytology in persons with HIV infection or HIV-negative MSM. More evidence is needed concerning the natural history of anal intraepithelial neoplasia, the best screening methods and target populations, safety of and response to treatments, and other programmatic considerations before screening can be routinely recommended. However, some clinical centers perform anal cytology to screen for anal cancer among high-risk populations (e.g., persons with HIV infection and MSM), followed by high-resolution anoscopy for those with abnormal cytologic results (e.g., ASC-US).