National Hernia Awareness Month is observed each June. Hernias can be described as abnormal bulges created by a weakness or a hole, usually in the abdominal wall or groin. It occurs when an internal organ, such as the bowel or bladder, extends through the wall of the muscle or tissue where it normally resides.
A bulge in the abdomen or groin caused by a hernia is a common condition in both men and women and can range from pain-free to painful. Nearly 1 million hernia operations are performed each year in the United States.
There are a number of places and types of hernias that can occur within the body.
- Abdominal Hernia – Also referred to as a ventral hernia, abdominal hernias are generally a protrusion that occurs above the belt. This happens due to a weakness in the abdominal wall.
- Hiatal Hernia – This type of hernia is closely connected & can coincide with a Paraesophageal Hernia, with the main symptom being gastric reflux or GERD. A hiatal hernia can commonly reoccur after surgery to repair it.
- Umbilical Hernia – Occurs around or in your belly button. If your belly button typically is pushed in, leaving an indent, and suddenly it appears to have a something bulging out then you most likely have an umbilical hernia.
- Incisional Hernia – Occurs at the incision line of a previous surgery, due to the cutting of the skin, tissue, & muscles in that particular area creating a weakened site.
- Femoral Hernia – Occurs at the top of the leg or groin area. These types of hernias are more common in women and tend to be recurrent after a hernia has been repaired.
- Inguinal Hernia –Occurs below the belt and on either side or both sides of the groin and/or the scrotum area. This particular hernia is more common in men and can also be recurrent, even after surgery.
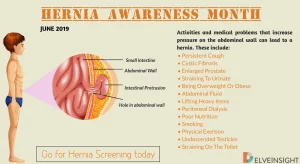
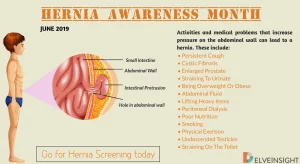
Hernias can be congenital, which means they were present at the time of birth. They can also develop due to tissue weakness in the abdominal wall or groin, usually from overexertion and straining. Long-term constipation issues or urinating, persistent cough, heavy lifting and physical exertion can all contribute to the development of hernias. Other factors that can increase your risk for hernias include poor nutrition, chronic obstructive pulmonary disease, obesity, pregnancy, previous surgeries (specifically open surgeries) and smoking.
When hernias become painful or symptomatic it may prevent patients from participating in work, exercise or other activities that they love to do. When a hernia becomes symptomatic it is important to see your primary care physician to discuss repair before the hernia becomes very large or turns into a very serious complication. When organs are stuck in a hernia, they can lose their blood supply, which may result in an emergency that requires immediate attention.
Many times, your physician will be able to diagnosis a hernia by physical exam. However, sometimes a hernia may be difficult to see or feel due to its location or a person’s body size and shape. In those instances, radiologic tests like a CT (computerized tomography) scan or ultrasound may be ordered to help with the diagnosis.
There are different options for surgical repair, including both open surgery and minimally invasive laparoscopic (using small incisions with a laparoscope) approaches. Many times, we utilize mesh to help repair the hernia to lower the recurrence risk. Hernia repair is usually performed under general anesthesia or on an outpatient basis, so patients may be able to go home on the same day of surgery.