How Cerebral Palsy is diagnosed:
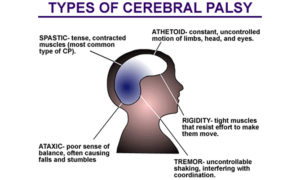
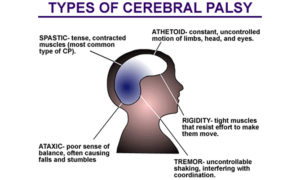
Most children with cerebral palsy are diagnosed during the first 2 years of life. But if a child’s symptoms are mild, it can be difficult for a doctor to make a reliable diagnosis before the age of 4 or 5. There are different types of CP affecting different muscle regions of the body. See above for details.
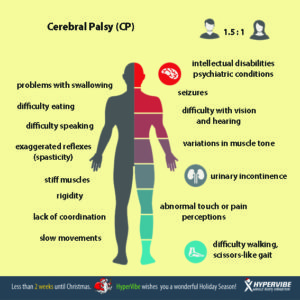
Doctors will order a series of tests to evaluate the child’s motor skills. During regular visits, the doctor will monitor the child’s development, growth, muscle tone, age-appropriate motor control, hearing and vision, posture, and coordination, in order to rule out other disorders that could cause similar symptoms. Although symptoms may change over time, CP is not progressive. If a child is continuously losing motor skills, the problem more likely is a condition other than CP—such as a genetic or muscle disease, metabolism disorder, or tumors in the nervous system.
Lab tests can identify other conditions that may cause symptoms similar to those associated with CP.
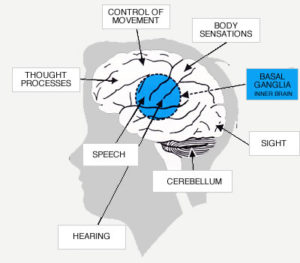
Neuroimaging techniques that allow doctors to look into the brain (such as an MRI scan) can detect abnormalities that indicate a potentially treatable movement disorder. Neuroimaging methods include:
- Cranial ultrasound uses high-frequency sound waves to produce pictures of the brains of young babies. It is used for high-risk premature infants because it is the least intrusive of the imaging techniques, although it is not as successful as computed tomography or magnetic resonance imaging at capturing subtle changes in white matter—the type of brain tissue that is damaged in CP.
- Computed tomography (CT) uses x-rays to create images that show the structure of the brain and the areas of damage.
- Magnetic resonance imaging (MRI) uses a computer, a magnetic field, and radio waves to create an anatomical picture of the brain’s tissues and structures. MRI can show the location and type of damage and offers finer levels of details than CT.
Another test, an electroencephalogram, uses a series of electrodes that are either taped or temporarily pasted to the scalp to detect electrical activity in the brain. Changes in the normal electrical pattern may help to identify epilepsy.
Some metabolic disorders can masquerade as CP. Most of the childhood metabolic disorders have characteristic brain abnormalities or malformations that will show up on an MRI.
Other types of disorders can also be mistaken for CP or can cause specific types of CP. For example, coagulation disorders (which prevent blood from clotting or lead to excessive clotting) can cause prenatal or perinatal strokes that damage the brain and produce symptoms characteristic of CP, most commonly hemiparetic CP. Referrals to specialists such as a child neurologist, developmental pediatrician, ophthalmologist, or otologist aid in a more accurate diagnosis and help doctors develop a specific treatment plan.
How is cerebral palsy treated?
Cerebral palsy can’t be cured, but treatment will often improve a child’s capabilities. Many children go on to enjoy near-normal adult lives if their disabilities are properly managed. In general, the earlier treatment begins, the better chance children have of overcoming developmental disabilities or learning new ways to accomplish the tasks that challenge them.
There is no standard therapy that works for every individual with cerebral palsy. Once the diagnosis is made, and the type of CP is determined, a team of health care professionals will work with a child and his or her parents to identify specific impairments and needs, and then develop an appropriate plan to tackle the core disabilities that affect the child’s quality of life. These following treatments are recommended by the FDA:
Physical therapy, usually begun in the first few years of life or soon after the diagnosis is made, is a cornerstone of CP treatment. Specific sets of exercises (such as resistive, or strength training programs) and activities can maintain or improve muscle strength, balance, and motor skills, and prevent contractures. Special braces (called orthotic devices) may be used to improve mobility and stretch spastic muscles.
Occupational therapy focuses on optimizing upper body function, improving posture, and making the most of a child’s mobility. Occupational therapists help individuals address new ways to meet everyday activities such as dressing, going to school, and participating in day-to-day activities.
Recreation therapy encourages participation in art and cultural programs, sports, and other events that help an individual expand physical and cognitive skills and abilities. Parents of children who participate in recreational therapies usually notice an improvement in their child’s speech, self-esteem, and emotional well-being.
Speech and language therapy can improve a child’s ability to speak, more clearly, help with swallowing disorders, and learn new ways to communicate—using sign language and/or special communication devices such as a computer with a voice synthesizer, or a special board covered with symbols of everyday objects and activities to which a child can point to indicate his or her wishes.
Treatments for problems with eating and drooling are often necessary when children with CP have difficulty eating and drinking because they have little control over the muscles that move their mouth, jaw, and tongue. They are also at risk for breathing food or fluid into the lungs, as well as for malnutrition, recurrent lung infections, and progressive lung disease.
Drug Treatments
Oral medications such as diazepam, baclofen, dantrolene sodium, and tizanidine are usually used as the first line of treatment to relax stiff, contracted, or overactive muscles. Some drugs have some risk side effects such as drowsiness, changes in blood pressure, and risk of liver damage that require continuous monitoring. Oral medications are most appropriate for children who need only mild reduction in muscle tone or who have widespread spasticity.
- Botulinum toxin (BT-A), injected locally, has become a standard treatment for overactive muscles in children with spastic movement disorders such as CP. BT-A relaxes contracted muscles by keeping nerve cells from over-activating muscle. The relaxing effect of a BT-A injection lasts approximately 3 months. Undesirable side effects are mild and short-lived, consisting of pain upon injection and occasionally mild flu-like symptoms. BT-A injections are most effective when followed by a stretching program including physical therapy and splinting. BT-A injections work best for children who have some control over their motor movements and have a limited number of muscles to treat, none of which is fixed or rigid.
- Intrathecal baclofen therapy uses an implantable pump to deliver baclofen, a muscle relaxant, into the fluid surrounding the spinal cord. Baclofen decreases the excitability of nerve cells in the spinal cord, which then reduces muscle spasticity throughout the body. The pump can be adjusted if muscle tone is worse at certain times of the day or night. The baclofen pump is most appropriate for individuals with chronic, severe stiffness or uncontrolled muscle movement throughout the body
Surgery
Orthopedic surgery is often recommended when spasticity and stiffness are severe enough to make walking and moving about difficult or painful. For many people with CP, improving the appearance of how they walk – their gait – is also important. Surgeons can lengthen muscles and tendons that are proportionately too short, which can improve mobility and lessen pain. Tendon surgery may help the symptoms for some children with CP but could also have negative long-term consequences. Orthopedic surgeries may be staggered at times appropriate to a child’s age and level of motor development. Surgery can also correct or greatly improve spinal deformities in people with CP. Surgery may not be indicated for all gait abnormalities and the surgeon may request a quantitative gait analysis before surgery.
Surgery to cut nerves. Selective dorsal rhizotomy (SDR) is a surgical procedure recommended for cases of severe spasticity when all of the more conservative treatments – physical therapy, oral medications, and intrathecal baclofen — have failed to reduce spasticity or chronic pain. A surgeon locates and selectively severs overactivated nerves at the base of the spinal column. SDR is most commonly used to relax muscles and decrease chronic pain in one or both of the lower or upper limbs. It is also sometimes used to correct an overactive bladder. Potential side effects include sensory loss, numbness, or uncomfortable sensations in limb areas once supplied by the severed nerve.
Assistive devices
Assistive devices such devices as computers, computer software, voice synthesizers, and picture books can greatly help some individuals with CP improve communications skills. Other devices around the home or workplace make it easier for people with CP to adapt to activities of daily living.
Orthotic devices help to compensate for muscle imbalance and increase independent mobility. Braces and splints use external force to correct muscle abnormalities and improve function such as sitting or walking. Other orthotics help stretch muscles or the positioning of a joint. Braces, wedges, special chairs, and other devices can help people sit more comfortably and make it easier to perform daily functions. Wheelchairs, rolling walkers, and powered scooters can help individuals who are not independently mobile. Vision aids include glasses, magnifiers, and large-print books and computer typeface. Some individuals with CP may need surgery to correct vision problems. Hearing aids and telephone amplifiers may help people hear more clearly.