The definition of heart failure, it occurs when the heart loses its ability to pump enough blood through the body. Usually, the loss in pumping action is a symptom of an underlying heart problem, such as hypertension and CAD = coronary artery disease. The term heart failure suggests a sudden and complete stop of heart activity but actually the heart does not suddenly or abruptly stop. Instead the way it works is heart failure usually develops over time, years. The heart first compensates with the disease or illness the individual has but, just like a car, after wear and tear the heart goes into decompensating to heart failure due to the heart decline. How serious is this condition? It varies from person to person depending on factors like an individual with obesity & unhealthy versus a person in healthier condition. All people diagnosed or not diagnosed with heart failure lose a pumping capacity of the heart happens as they age but diagnosed with heart failure makes the engine of the body a challenge in doing its function properly. The pump loss is more significant in the person with heart failure and often results from a heart attack (actual scaring to the tissue=death to that tissue area) or from other diseases that can damage the heart. The severity of the condition determines the impact it has on a person’s life. At the other end, extremes, treatment often helps people lead full lives if the person follows the meds ordered by the doctor including the diet and activity/exercise the doctor orders to the patient with heart failure (compliance so important). There are different levels of heart failure but even the mildest form is a serious health problem, which must be treated. If not the pump (the heart) will just get worse in doing its function properly. To improve the chance of living longer in an individual with heart failure, patients must take care of themselves, see their physician (cardiologist) on a regular basis, and closely follow treatments (as ordered) with knowing what heart failure actually to understanding how the disease works (is the failure on the right side or left side? Which in time will effect the other side in time). In knowing what side the failure is on will make you understand what signs and symptoms to expect.
Types of Heart Failure
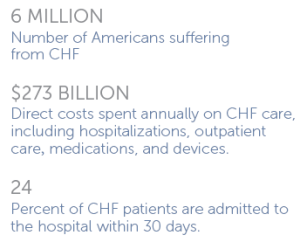
The term congestive heart failure (CHF) is often used to describe all patients with heart failure. In reality, congestion=the buildup of fluids in the heart for not pumping correctly, just like pipes in a home not working properly=back up of water in the pipes, happens with CHF also to the fluids (blood) backing up in the lungs. This is just one feature of the condition and does not occur in all patients. There are two main categories of heart failure although within each category, symptoms and effects may differ from patient to patient. The two categories are:
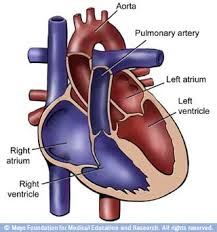
1-Systolic heart failure (systolic is the top number of your blood pressure=the heart at work). This occurs when the heart’s (muscle-myocardium) ability to contract (pump=being active) decreases, particularly starting on the L side of the heart where the muscle of the heart is greatest (myocardium=heart muscle). The heart cannot pump blood with enough force to push a sufficient amount out of the heart into the circulation through the aorta. The aorta is a artery (vessel) that leaves the L lower chamber of the heart (left side of the heart=highly oxygenated rich blood). Due to the heart not using enough force pushing the blood forward in the aorta this causes the blood to back up and cause it to go back up into the L lower to the L upper chamber that goes further back up into the pulmonary vein into the lungs=congestion in the lungs due to the heart failure.
2-Diastolic heart failure (diastolic is the bottom number of your blood pressure which is the pressure when the heart is at rest). This failure occurs when the heart has a problem relaxing. The heart cannot properly fill with blood because the muscle of the heart due to trying so hard to compensate over a long period of time with disease (ex. High B/P, Obesity, etc…) strains the heart in doing its function that failure finally starts that the muscle of the heart (myocardium) becomes stiff. This causes the heart to lose its ability to relax to allow proper filling of the heart in upper and lower chambers=back up of the blood. This failure starts on the right side of the heart causing the blood to back up away from the heart and may lead this blood that is highly concentrated with carbon dioxide to accumulation especially in the feet, ankles and legs. Some patients may have lung congestion.
Causes of Heart Failure:
As stated, the heart loses some of its blood pumping ability as a natural consequence of aging. How- ever, a number of other factors can lead to a potentially life-threatening loss of pumping activity.
As a symptom of underlying heart disease, heart failure is closely associated with the major risk factors for coronary heart disease: smoking, high cholesterol levels, hypertension (persistent high blood pressure), diabetes= abnormal blood sugar levels, and obesity. A person can change or eliminate those risk factors and thus lower their risk of developing or aggravating their heart disease and heart failure through healthy habits performed routinely, proper dieting, and balancing rest with exercise.
Among prominent risk factors, hypertension-HTN (high blood pressure) and diabetes are PARTICULARLY IMPORTANT. Uncontrolled HTN increases the risk of heart failure by 200 %, compared to those who do not have hypertension. Moreover, the degree of risk appears directly related to the severity of the high blood pressure.
Persons with diabetes have about a two to eight fold greater risk of heart failure than those without diabetes. Women with diabetes have a greater risk of heart failure than men with diabetes. Part of the risk comes from the diabetes association with other risk factors for heart disease such as high cholesterol or obesity or other risk factors. However, the disease process of diabetes also damages the heart muscle.
The presence of coronary disease is among the greatest risks for heart failure. Muscle damage and scarring caused by a heart attack greatly increase the risk of heart failure. Cardiac arrhythmias, or irregular heartbeats, also raise heart failure risk. Any disorder that causes abnormal swelling or thickening of the heart sets the stage for heart failure.
In some people, heart failure arises from problems with heart valves, the flap-like structures that help regulate blood flow through the heart. Infections in the heart are another source of increased risk for heart failure.
A single risk factor may be sufficient to cause heart failure, but a combination of factors dramatically increases the risk. Advanced age adds to the potential impact of any heart failure risk.
Finally, genetic abnormalities contribute to the risk for certain types of heart disease, which in turn may lead to heart failure. However, in most instances, a specific genetic link to heart failure has not been identified.
SO LIVE AS HEALTHY AS POSSIBLE IN YOUR ROUTINE HABITS, YOUR DIETING OF THE 4 FOOD GROUPS, MAINTAINING YOUR WEIGHT IN A THEREPEUTIC RANGE (look as calculating BMI online for free to find out what your weight range for your height is), and BALANCING REST WITH EXERCISE TO HELP DECREASE THE CHANCE OF GETTING HEART FAILURE. Go to healthyusa.tsfl.com to learn what Dr. Anderson through his book of “Dr. A.’s Healthy Habits” and many other mentors in directing a healthy life; just research it.
CHF part 2 tomorrow and learn what the signs and symptoms with how its diagnosed, how its treated with tips on the disease (most importantly prevention).