1.) Binge Eating
Binge Eating Disorder (BED) is newly-recognized and is characterized by recurrent episodes of binge eating that occur twice weekly or more for a period of at least six months. During bingeing, a larger than normal amount of food is consumed in a short time frame and the person engaging in the bingeing behavior feels a lack of control over the eating.
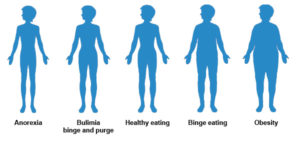
In BED, bingeing episodes are associated with at least three characteristics such as eating until uncomfortable, eating when not physically hungry, eating rapidly, eating alone for fear of being embarrassed by how much food is being consumed, or feeling disgusted, depressed or guilty after the episode of overeating. These negative feelings may in turn trigger more bingeing behavior. In addition, although BED behaviors may cause distress by those affected, it is not associated with inappropriate compensatory behaviors such as those found in Bulimia Nervosa or Anorexia Nervosa. Therefore, people with BED often present as either overweight or obese because they consume so many extra calories.
2.) Anorexia Athletica
Anorexia Athletica is a constellation of disordered behaviors on the eating disorders spectrum that is distinct from Anorexia Nervosa or Bulimia Nervosa. Although not recognized formally by the standard mental health diagnostic manuals, the term Anorexia Athletica is commonly used in mental health literature to denote a disorder characterized by excessive, obsessive exercise. Also known as Compulsive Exercising , Sports Anorexia, and Hypergymnasia, Anorexia Athletica is most commonly found in pre-professional and elite athletes, though it can exist in the general population as well.
People suffering from Anorexia Athletica may engage in both excessive workouts and exercising as well as calorie restriction. This puts them at risk for malnutrition and in younger athletes could result in endocrine and metabolic derangements such as decreased bone density or delayed menarche.
Symptoms of Anorexia Athletica may include over-exercising, obsession with calories, fat, and weight, especially as compared to elite athletes, self-worth being determined by physical performance, and a lack of pleasure from exercising. Advanced cases of Anorexia Athletica may result in physical, psychological, and social consequences as sufferers deny that their excessive exercising patterns are a problem.
3.) Over Exercise
“Over exercise” is a general term referring to exercising to the point of exhaustion. Over exercise can occur once in a while as when someone overdoes it on a single work-out, or it can be a habitual behavior. When over exercising becomes the norm, this may be an indication that a person is actually suffering from what is called Obligatory Exercising, Compulsive Exercising, or Anorexia Athletica. When someone over exercises to the point where it is a problem, he or she may experience physical, psychological and social consequences.
4.) Overeating
Overeating is not a specific diagnosis of any sort but may rather refer to a discrete incident of eating too much such as during holidays, celebrations, or while on vacation, or it may refer to habitual excessive eating.
People who engage in overeating regularly tend to eat when not hungry and may eat alone because they are embarrassed about the portions of food they are consuming. In addition, they may spend exorbitant amounts of time fantasizing about their next meal. Another sign that overeating has become a problem is if excessive amounts of money are wasted on food. In general, people who overeat are overweight or obese though people with normal body weights may overeat from time to time as well.
Overeating becomes problematic when it manifests as a compulsive or obsessive relationship with food. At this point it may be treated with behavior modification therapy or as a food addiction. One program available that supports people in recovering habitual, problematic overeating using the context of an addiction is Overeaters Anonymous (OA). OA is set up similarly to Alcoholics Anonymous (AA) and is a twelve step program in which members acknowledge that they are powerless over food. OA is open to anyone who has an unhealthy relationship with food and who wishes to stop.
5.) Night Eating
Night Eating Syndrome (NES) is an emerging condition that is gaining increased recognition among medical professionals. Its clinical importance is in relation to obesity as many people who suffer from NES are overweight or obese and being overweight or obese comes with many negative health risks. Although not classified as one of the types of eating disorders, as a syndrome, NES is considered a constellation of symptoms of disordered eating characterized most prominently by a delayed circadian timing of food intake.
People with NES tend to not eat in the morning and consume very little during the first half of the day. The majority of their calories are then consumed in the evening hours, so much so that sleep may be disturbed so that a person can eat. People with NES may be unable to get back to sleep after eating or may experience frequent awakenings throughout the night for feedings. However, people with NES are fully awake and aware of their eating episodes.
It is distinct from bingeing disorders in that the portions consumed are generally those of snacks rather than huge meals. In addition, it differs from Bulimia Nervosa since there are no compensatory or purging behaviors present to offset increased calorie intake.
6.) Orthorexia
Orthorexia Nervosa (also known as “orthoexia”) is a term coined by physician Steven Bratman in an article he wrote for Yoga Journal in 1997. It is not a traditionally recognized type of eating disorder but it does share some characteristics with both Anorexia Nervosa and Bulimia, most specifically obsession with food.
Orthorexia refers to a fixation on eating “pure” or “right” or “proper” food rather than on the quantity of food consumed.
Having Orthorexia Nervosa is like suffering from Workaholism or Exercise Addiction in which something that is normally considered good or healthy is done in excess and to the point that a person becomes obsessed with the activity. Like other obsessive disorders people with Orthorexia Nervosa experience cyclical extremes, changes in mood, and isolate themselves. Most of their life is spent planning and preparing meals and resisting temptation to the exclusion of other activities. They may even go to the extreme of avoiding certain people who do not share in their dietary beliefs or carry their own supply of food wherever they go.
Like other eating disorders, Orthorexia Nervosa may result in negative consequences. Social isolation, physical deterioration, and a failure to enjoy life can occur. There have even been a few deaths related to Orthorexia Nervosa when a person becomes so low in body weight due to restrictive eating or fasting that the heart fails.
7.) EDNOS – Eating Disorder Not Otherwise Specified
According to the Diagnostic and Statistical Manual, 4th Edition there exists a category of eating disorders that do not meet the specific criteria for the two defined disorders, Anorexia Nervosa and Bulimia. When people exhibit behaviors in the spectrum of disordered eating but do not meet all the criteria for Anorexia Nervosa or Bulimia, they are given a diagnosis of an Eating Disorder Not Otherwise Specified (EDNOS). Over one-half to two-thirds of people diagnosed with eating disorders fall into the category of EDNOS. More people are diagnosed with EDNOS than Anorexia Nervosa and Bulimia combined.
Binge Eating Disorder (BED) is the only type of eating disorder under the category of EDNOS. A person meets the definition of having EDNOS if they have exhibit all the criteria for Anorexia Nervosa but have regular menstruation or a normal body weight, or if they exhibit all the criteria for Bulimia but purge less than two times per week or for a duration shorter than three months, or if only small amounts of food are purged, or if a person spits out food rather than swallowing it.
People diagnosed with EDNOS can experience the same negative psychological, social, and physical consequences as a person diagnosed with Anorexia Nervosa or Bulimia. The seriousness of their condition is no different than that for people diagnosed with specific disorders. The only difference is that the person may experience a spectrum of disordered eating behaviors and these behaviors may change over time.
Although BED is the only one of the types of eating disorders categorized under EDNOS, people who are considered to have Sub Therapeutic Anorexia Nervosa or Sub Therapeutic Bulimia are also given a diagnosis of EDNOS. To have Sub Therapeutic Anorexia Nervosa or Bulimia means that a person displays some but not all of the criteria for the full-blown condition.