Listed below are some of the most common illnesses to watch out for during the holiday season, including a few tips to assist with prevention.
1.) The Common Cold
There are many viruses that can cause the common cold, all with similar symptoms, including: nasal congestion, sore throat, cough, headache, and sometimes fever. While a cold can occur any time of the year, the common cold rears its stuffy head most often during the winter months. There is no cure for the common cold, but rest, hydration and nutrition will help you feel better as your body works through the healing process. Most colds reach the peak of their severity between three and five days of symptom onset, with resolution in about a week.
2.) The Flu
The flu is often mistaken for the common cold. Flu tends to present quickly and severely. Coughing, sore throat, headaches, body aches and high fever, are common flu symptoms. If you develop flu-like symptoms, take fever reducing medication and see your healthcare provider. To assist with prevention, we recommend that everyone in your family receive an annual flu shot.
3.) RSV and Bronchiolitis
Respiratory Syncytial Virus (RSV) is a common virus that usually causes mild, cold-like symptoms, including nasal congestion, cough, fever, wheezing and dehydration. RSV is a significant cause of respiratory illness in young children and older adults. RSV can last one or two weeks and has the potential of becoming serious. In the United States, RSV is the most common cause of bronchitis and pneumonia in children younger than 12 months. Seek medical attention if you or your child have trouble breathing. To avoid spreading the infection, disinfect surfaces and wash your hands regularly.
4.) Strep Throat
Strep throat is a bacterial infection caused by group A Streptococcus and is most common among school-age children. In addition to a sore throat, symptoms can include pain when swallowing, fever, red and swollen tonsils, tiny red spots on the roof of the mouth, and enlarged lymph nodes in the front of the neck. Your doctor can do a swab test to determine if group A strep bacteria is the cause of your sore throat. If positive, antibiotics will be prescribed to help heal the infection, prevent future serious health problems, and avoid spreading the infection to others. Prevent close contact, disinfect surfaces and wash hands regularly to prevent spreading the infection.
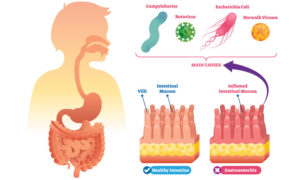
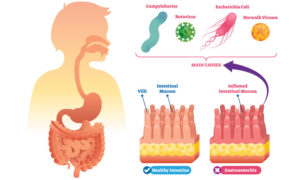
5.) Norovirus
Norovirus is a very contagious and common stomach bug that can lead to severe vomiting and diarrhea. Though it can strike at any time of the year, it’s most commonly passed around during the winter months. Common nicknames for the Norovirus is “winter vomiting bug” and “stomach flu”. If you contract a stomach bug, make sure to drink plenty of fluids to prevent dehydration and seek medical attention if not able to keep fluids down. Symptoms tend to last two to three days. If someone in your family has the norovirus, keep interactions limited and wash your hands regularly.
Prevention is the Best Medicine
It is always important to practice good hygiene, especially when you or those around you are sick. Make sure to wash your hands thoroughly, cover your cough, stay hydrated, and maintain a healthy immune system through proper nutrition. While most of these common illnesses will run their course without any intervention, you should see a doctor immediately if your symptoms worsen.
From striveforgoodhealth’s family to yours, we wish you a safe and happy holiday season (woof!).